Preventive Care in Nursing and Midwifery Journal

Volume 14, Issue 4 (10-2024)
Prev Care Nurs Midwifery J 2024, 14(4): 13-23 |
Back to browse issues page
Ethics code: IR.ZUMS.REC.1400.496
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Gholamian E, Hanifi N, Shiri Qidari P. Treatment selection factors and outcome comparison in acute myocardial infarction. Prev Care Nurs Midwifery J 2024; 14 (4) :13-23
URL: http://nmcjournal.zums.ac.ir/article-1-931-en.html
URL: http://nmcjournal.zums.ac.ir/article-1-931-en.html
Department of Emergency and Critical Care, School of Nursing and Midwifery, Zanjan University of Medical Sciences, Zanjan, Iran , nasrinhanifi@zums.ac.ir
Full-Text [PDF 978 kb]
(562 Downloads)
| Abstract (HTML) (1324 Views)
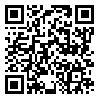
Figure 1.
Study diagram
Results
Out of 340 patients with STEMI in this study, 88 were excluded due to receiving treatment elsewhere or incomplete medical records. The data of 252 patients with STEMI was finally analyzed. In the present study, the most common primary therapeutic intervention was PPCI (45.6 %). Thrombolytic therapy was the initial treatment for 35.3% of patients. Thrombolytic therapy was unsuccessful in 41.1% of patients and these patients underwent PCI Rescue. Only heparin and nitroglycerin were used for 19% of patients in the initial stage with no intervention.
Based on Table 1, the ANOVA test showed that there was a statistically significant difference in mean age between the treatment groups. In a pairwise comparison of groups, the no-intervention group had a significantly higher mean age than the thrombolytic therapy group (p=0.032) and the PPCI group (p=0.014). However, the mean age did not differ significantly between the two groups of thrombolytic therapy and PPCI (p>0.05). The gender distribution in various treatment groups showed significant differences (p=0.02). PPCI was the most common treatment for male patients. The average vital signs) include: systolic/diastolic blood pressure, heart rate, respiratory rate and Oxygen saturation (and Killip score did not show a statistically significant difference across various treatment groups (p>0.05). The time it took for the group with no intervention to reach the hospital differed significantly from the PPCI and thrombolytic therapy groups (p=0.0001). The time from hospital arrival to treatment initiation was significantly longer in the no-intervention group compared to the PPCI and thrombolytic therapy groups (p=0.0001). The PPCI group experienced a significantly longer delay between hospital arrival and treatment initiation compared to the thrombolytic therapy group (p=0.005). The groups showed significant differences in average pain levels before and after blood reperfusion, with the no-intervention group experiencing less pain before blood reperfusion than the PPCI and thrombolytic therapy group (p<0.001). The pain post-reperfusion was significantly lower in the PPCI and no intervention groups compared to the thrombolytic therapy group (p<0.001) (Table 1).
* Fishers exact test; **Chi-square
The hospitalization cost in the PPCI group was higher than the thrombolytic therapy group and the no-intervention group, but the difference was not statistically significant (p=0.213). The no-intervention group had a longer average hospitalization than the PPCI and thrombolytic groups, and this difference was statistically significant (p=0.033). Nonetheless, there was no difference in hospitalization duration between the two groups of thrombolytic therapy and PPCI (p=0.887). There was a higher average of analgesia prescriptions in the thrombolytic therapy group compared to the PPCI and the no-intervention group, although this was not statistically significant (p=0.592). In comparison to the PPCI and thrombolytic therapy group, the no-intervention group had higher one-year mortality. This difference was not statistically significant (p=0.085). The thrombolytic group had a higher rate of re-hospitalization within one year compared to the PPCI and the no-intervention group, but the difference was not significant (p=0.083).
Discussion
Studies have proven the superiority of PPCI over thrombolytic therapy for STEMI patients hospitalized within the golden period [14,16,17, 36], but this method requires special facilities, and the number of centers providing this technique are limited [20]. Achievement of reperfusion via PPCI with an experienced operator in the "golden time" in many countries is a problematic issue [35]. Parts of Iran face limitations that make it challenging to achieve a 24.7 environment for PPCI. The patient's condition may prevent PPCI intervention. The purpose of this study is twofold: first, to identify factors influencing the choice of myocardial infarction treatment that can help remove barriers to PPCI. Second, to compare myocardial infarction treatment methods so that, in the absence of differences in treatment outcomes, thrombolytic therapy can be an alternative to PPCI in certain uncorrectable conditions. Therefore, this study designed to determine treatment selection factors and outcomes in acute cardiac infarction patients.
The no-intervention group had a higher average age than the thrombolytic therapy and PPCI group in the current study. Young patients often underwent PPCI or thrombolytic therapy for timely referral to medical centers. late presentation to the hospital of neglected MI in older patients, who did not receive primary intervention, resulted in missed opportunities for blood reperfusion. Young patients were more familiar with the symptoms of myocardial infarction and the complications of not treating it promptly than older patients, so they were referred to medical centers more quickly and had a greater chance of receiving reperfusion therapy. There was no statistical difference in the average age of the PPCI and thrombolytic therapy groups in some studies [34,37-39]. In a study, the thrombolytic therapy group had a lower average age compared to the PPCI group [35]. There was no study that compared the average age in the no-intervention group with the thrombolytic therapy and PPCI group.
In the present study, male patients mostly received PPCI, whereas, in Soleimani et al.'s study, men were mostly treated with thrombolytic therapy [35]. Treatment selection based on gender had no significant difference in other studies [34, 38,40]. Thrombolytic therapy was administered to the majority of smoking patients in the study, in line with Soleimani et al.'s findings [35]. Similar to previous studies, the finding of the present study revealed no significant difference in mean vital signs and Killip score within the selected treatment group [17,20,31,40].
Patients were primarily treated with PPCI based on the availability of a 24/7 operational catheterization lab and an interventional cardiologist and written informed consent patient. In the case of spontaneous reperfusion, failure to diagnose STEMI on time, or Neglected MI, patients might not receive immediate intervention and instead were given routine medications like heparin and nitroglycerin. Thrombolytic therapy was the primary treatment for patients admitted on holidays. The Likelihood Ratio test in regression analysis demonstrated that catheterization lab activity and interventional cardiologist availability predicted treatment selection. the present study showed that younger individuals (patients aged 32-52 compared to patients over 73) were more likely to be considered for PPCI, although Killip's classification did not play a role in the decision of primary treatment. Aging, chronic renal failure, and higher Killip classification were negatively correlated with PPCI and thrombolytic therapy in some studies [24,41].
Similar to Pu et al.'s study [17], in the present study among the mechanical complications of STEMI only the incidence of hematuria was significantly associated with the type of initial intervention, so the incidence of this complication was higher in the thrombolytic group. In line with prior studies, there was no statistically significant difference in other mechanical complications between the treatment groups [34,39,40].
Khan et al.'s study found that the thrombolytic therapy group had a significantly higher rate of stroke, recurrent myocardial infarction, and heart failure compared to the PPCI group [42], which goes against the results of the present study. The potential reason for the difference between the results of the current study and the above-mentioned research could be the effect of age on patient outcomes, since older patients may have more underlying diseases, which in turn can increase complications rate; accordingly, studies including patients within different age groups could have different complications rates following PCI or thrombolytic therapy. In Khan et al.'s study, the mean age of the thrombolytic group was higher than the PPCI group, which could be responsible for the higher incidence of complications in this group. Similar to a previous study, the treatment groups did not show a significant difference in the electrical complications caused by STEMI [35]. Only the incidence of cardiac arrest was higher in the PPCI group than in the other two groups.
The duration of hospitalization was much longer for the group that did not receive initial intervention, in contrast to both the PPCI group and the thrombolytic therapy group. However, there was no difference in the length of hospital stay between the thrombolytic therapy and PPCI groups. Therefore, it can be concluded that patients who did not receive initial intervention had a longer hospital stay. According to Kazemi et al, the thrombolytic therapy and PPCI groups had the same hospital stay duration [40]. The data suggests that the group receiving no intervention had a relatively higher mortality rate after one year when compared to the PPCI and thrombolytic treatment groups. Nevertheless, this distinction did not show statistical significance, which is consistent with the results of previous research [17,31,34, 35,37,39].
A notable strength of this study was its analysis of treatment factors and outcomes across three groups: PPCI, thrombolytic therapy, and no intervention. The study's retrospective approach restricts access to accurate information, highlighting the importance of future prospective studies.
Conclusion
Addressing barriers is crucial to promote timely PPCI over thrombolytic therapy. In countries where achieving the "golden time" for PPCI treatment is difficult, thrombolytic therapy followed by rescue PCI is a highly effective alternative. The study revealed that there were no significant differences in complications, clinical outcomes, mortality, and rehospitalization between patients who underwent PPCI and those treated with thrombolytic therapy. Thus, thrombolytic therapy remains a viable alternative when timely PPCI treatment cannot be achieved. Patients who couldn't receive PPCI for any reason might be stressed about not receiving their preferred treatment. Thrombolytic therapy's effectiveness can be reinforced by the findings of this study.
Ethical Consideration
The ethics committee of Zanjan University of Medical Sciences granted permission for the research, registered as IR.ZUMS.REC.1400.496. By presenting a written letter of introduction from the Research Vice-Chancellor of Zanjan University of Medical Sciences, the researcher was introduced to the directorate of Ayatollah Mousavi Hospital. Before conducting the research, the officials were informed about its purpose and nature to secure their cooperation. Officials were assured that patient information would be confidential, and when reviewing patient records, they would omit patient characteristics and identity details.
Acknowledgments
The authors appreciate the support of the staff of Ayatollah Mousavi Hospital.
Conflict of interest
The authors declares they have no conflict of interest.
Funding
The Research and Technology Vice-Chancellor of Zanjan University of Medical Sciences has funded this project.
Authors' contributions
Hanifi N., Gholamian E., and Shiri Ghidari P. were responsible for the study design. Gholamian E. gathered the data. All authors were responsible for statistical analysis and interpretation of the data, drafting of the manuscript, and critical revision of the manuscript.
Artificial Intelligence Utilization
The authors did not use any Artificial Intelligence (AI) tools or technologies during the preparation of this manuscript.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to privacy restrictions but are available from the corresponding author upon reasonable request.
Full-Text: (142 Views)
Introduction
Acute Myocardial Infarction (AMI) annually affects 1.2 million people worldwide, making it a leading cause of hospitalization and death [1,2]. Patients and the healthcare system bear a heavy economic burden due to the costs of diagnosing, treating, and re-admitting patients with myocardial infarction [3]. Ibanez cites the WHO as reporting that 50% of deaths in developed countries and 30% in developing countries are caused by myocardial infarction [4]. According to a UK national self-reporting survey in 2014, the prevalence of MI was reported as 640,000 in men and 275,000 in women [5]. The age-specific prevalence of MI extends from 0.06% of men <45 years old to 2.46% of those ≥75 years. In contrast to these developed countries, South Asian countries (India, Pakistan, Sri Lanka, Bangladesh, and Nepal) have the highest prevalence of MI seen in those younger than 45 years of age compared to those older than 60 years [6]. The recent estimates of the incidence of MI in the USA are about 525,000 based on AHA data [7]. Because of improved health systems and effective public health strategies, the rates are surging in developing countries such as South Asia, parts of Latin America, and Eastern Europe [6]. AMI has increased 12 times in women and almost 14 times in men from 1990 to 2020 in developing countries like Iran [8]. Sharif Nia et al., citing the Iranian Ministry of Health, Treatment and Medical Education report that 39.3% of deaths are caused by heart diseases, with 19.5% specifically attributed to AMI [9]. Eliminating death from cardiovascular disease in Iran could boost life expectancy by 1.23 years [10].
STEMI is known as an emergency cardiovascular disease, which should be quickly identified and treated to ensure optimal results [11,12]. Immediate reperfusion is the standard treatment for a patient with STEMI [4]. In the treatment of STEMI, there are two methods used to restore blood flow in the blocked vessel: Primary Percutaneous Coronary Intervention (PPCI) (mechanical re-opening) or thrombolytic (medical re-opening) [13]. PPCI is the preferred choice for reperfusion in STEMI when done on time and by a skilled team [14-17].
However, in some circumstances, PPCI is not an immediate option and thrombolysis could be initiated expeditiously [4]. In fact, despite better clinical outcomes seen in the case of PPCI, in the majority of patients who do not have access to PPCI, thrombolytic therapy is offered as the selective treatment for reperfusion [18]. Since many hospitals do not have the resources to provide PPCI, a large proportion of STEMI patients go to larger hospitals for PPCI. Transmission for PPCI involves a longer delay in treatment, resulting in a loss of potential gain compared to receiving drugs in local hospitals [19]. Treatment using venous thrombolysis is more accessible and less dependent on the geographical situation and available facilities [20]. Delays from the onset of pain to treatment can also affect the choice of treatment type [21]. The efficacy of thrombolytic agents is highly time-dependent [22]. Thrombolysis showed no benefit in patients with STEMI when administered between 12 and 24 hours after the onset of chest pain [23]. Weaker recommendations are given for PPCI 12-24 hours after symptom onset in the absence of ongoing ischemia [21]. PPCI is not applied to all AMI patients because of concurrent factors related to patient and/or medical institutional background [24]. In particular, older patients with AMI often have multiple comorbidities and physical disabilities [25,26] which might have negative effects on decisions regarding PPCI made by general or interventional cardiologists [24]. Other patient populations at risk for disparities include those with diabetes and those with chronic kidney disease [27]. Clinical variables such as higher age, female sex, and higher Killip class (The Killip classification was introduced for clinical assessment of patients with acute MI, and it stratifies individuals according to the severity of their post-MI HF [28]), and renal dysfunction, but not functional status on admission, were predictors of non-application of PPCI [24].
Regarding the above, the decision on how to treat STEMI patients is always difficult due to numerous influencing factors. There are several reasons and factors underlying the choice of reperfusion treatment, such as the Patient's age, gender, Killip class, underlying diseases, and late referral to the medical center due to lack of familiarity with the symptoms of myocardial infarction, etc. [24,25,27,29]. Some of these factors that influence treatment choices can be controlled by preventive nursing measures. For example, in late referral to the medical center, a policy should be adopted to provide the necessary information to the community by providing training courses to specific population groups on the symptoms of myocardial infarction and the need for prompt treatment. How to deal with a person with chest pain, avoiding wasting time, and quickly contacting the emergency room are the main pillars of treating this disease. If an emergency room is not available, the community should be aware of centers equipped with treatment facilities and get to these centers as soon as possible. These matters depend to a large extent on the education and awareness of the community, and increasing public awareness, whether through promotional displays and posters or through lectures and workshops, can be very effective in this regard. In Iran, no study was found that investigated the influencing factors in choosing the treatment of myocardial infarction. Assessing these factors can help overcome barriers to preferred STEMI treatment. In addition, by analyzing and comparing the side effects and outcomes of various treatment approaches, the effectiveness of thrombolytic therapy can be ensured to be a suitable alternative treatment to PPCI in specific circumstances.
Objectives
This study aimed to determine treatment selection factors and outcomes in acute cardiac infarction patients.
Methods
This cross-sectional and retrospective study examined the data of 252 myocardial infarction patients referred to Ayatollah Mousavi Hospital from April 2021 to March 2022 (Fig. 1).
Ayatollah Mousavi Hospital is a specialized center for heart services in Zanjan province. Code 247 is used for treating MI patients in the province. The telephone triage unit promptly responds to the patient's EMS call as per Code 247 policy. An electrocardiography (ECG) is taken immediately from the patient and sent to a specialist after the ambulance is dispatched. Code 247 is activated with an initial MI diagnosis, notifying the target hospital and the supervisor. Patients with ST-elevation MI are sent to the angiographic unit, whereas those with non-ST-elevation MI are referred to an emergency medicine specialist. However, STIM patients may not always be sent to the angiography department for various reasons.
Based on a study by Hanifi et al. [30], the minimum sample size of 196 people for sampling adequacy was estimated considering a standard deviation of 140 minutes for the time to treatment, a sampling error of 20 minutes, a power of 80%, and a confidence level of 95%. Convenience sampling was utilized in the present study. The medical records of all patients diagnosed with STEMI were thoroughly reviewed from April 1st, 2021 to March 31st, 2022. Out of the 340 patients diagnosed with STEMI, a total of 252 eligible patients were carefully chosen and their information was thoroughly analyzed. The medical records of patients with a diagnosis of STEMI (as determined by clinical symptoms, electrocardiogram changes, and elevated cardiac enzymes by the American College of Cardiology (ACC) and the American Heart Association (AHA) guidelines [31]) were selected for inclusion in the study. Study exclusion criteria were medical records of patients who had received thrombolytic therapy at another center before being referred to Ayatollah Mousavi Hospital and medical records with incomplete information.
The variables studied in this research were:
1. The possible determining factors for choosing the primary treatment intervention
2. Success or failure of treatment (Treatment success is determined by ST-Elevation removal of at least 50% in ECG or relief of chest pain within 90 minutes.)
3. Mechanical and electrical complications following treatment
4. Clinical outcomes (hospitalization cost, length of hospital stay, number of painkiller prescriptions),
5. One-year death rate and readmission due to heart problems within one year
The checklist used for data collection was prepared by reviewing past evidence and expert professors of the intensive care unit of the Zanjan School of Nursing and Midwifery opinions. The checklist was created by consulting trustworthy scientific literature [31-35]. Instrument validity was assessed using content validity. The designed instrument was presented to 10 experts (Professors and nurses with experience in the field of coronary care), and necessary changes were made according to their opinions. The reliability of the instrument was checked using inter-rater agreement. Both researchers completed the designed tool for ten patients to ensure reliability. The Kappa agreement coefficient between the two researchers was 95%.
Descriptive statistics were employed for data analysis, utilizing the mean and standard deviation for quantitative variables and frequency and percentage for qualitative variables. The normality of the data was assessed by analyzing the data's skewness and kurtosis. The Chi-square test/Fisher's exact test was utilized to assess the possible factors correlated with the selection of treatment intervention. Multiple logistic regression analysis was used to analyze the selection of primary intervention for reperfusion and identify associated predictors. Analysis of variance was utilized to assess and contrast clinical outcomes across diverse treatment groups. Furthermore, The Chi-square test/Fisher's exact test was utilized to compare the incidence of mechanical and electrical complications, readmission rates, and one-year mortality among the treatment groups for STEMI. Statistical analyses were conducted using SPSS version 22 software with a significance level set at 0.05.
Acute Myocardial Infarction (AMI) annually affects 1.2 million people worldwide, making it a leading cause of hospitalization and death [1,2]. Patients and the healthcare system bear a heavy economic burden due to the costs of diagnosing, treating, and re-admitting patients with myocardial infarction [3]. Ibanez cites the WHO as reporting that 50% of deaths in developed countries and 30% in developing countries are caused by myocardial infarction [4]. According to a UK national self-reporting survey in 2014, the prevalence of MI was reported as 640,000 in men and 275,000 in women [5]. The age-specific prevalence of MI extends from 0.06% of men <45 years old to 2.46% of those ≥75 years. In contrast to these developed countries, South Asian countries (India, Pakistan, Sri Lanka, Bangladesh, and Nepal) have the highest prevalence of MI seen in those younger than 45 years of age compared to those older than 60 years [6]. The recent estimates of the incidence of MI in the USA are about 525,000 based on AHA data [7]. Because of improved health systems and effective public health strategies, the rates are surging in developing countries such as South Asia, parts of Latin America, and Eastern Europe [6]. AMI has increased 12 times in women and almost 14 times in men from 1990 to 2020 in developing countries like Iran [8]. Sharif Nia et al., citing the Iranian Ministry of Health, Treatment and Medical Education report that 39.3% of deaths are caused by heart diseases, with 19.5% specifically attributed to AMI [9]. Eliminating death from cardiovascular disease in Iran could boost life expectancy by 1.23 years [10].
STEMI is known as an emergency cardiovascular disease, which should be quickly identified and treated to ensure optimal results [11,12]. Immediate reperfusion is the standard treatment for a patient with STEMI [4]. In the treatment of STEMI, there are two methods used to restore blood flow in the blocked vessel: Primary Percutaneous Coronary Intervention (PPCI) (mechanical re-opening) or thrombolytic (medical re-opening) [13]. PPCI is the preferred choice for reperfusion in STEMI when done on time and by a skilled team [14-17].
However, in some circumstances, PPCI is not an immediate option and thrombolysis could be initiated expeditiously [4]. In fact, despite better clinical outcomes seen in the case of PPCI, in the majority of patients who do not have access to PPCI, thrombolytic therapy is offered as the selective treatment for reperfusion [18]. Since many hospitals do not have the resources to provide PPCI, a large proportion of STEMI patients go to larger hospitals for PPCI. Transmission for PPCI involves a longer delay in treatment, resulting in a loss of potential gain compared to receiving drugs in local hospitals [19]. Treatment using venous thrombolysis is more accessible and less dependent on the geographical situation and available facilities [20]. Delays from the onset of pain to treatment can also affect the choice of treatment type [21]. The efficacy of thrombolytic agents is highly time-dependent [22]. Thrombolysis showed no benefit in patients with STEMI when administered between 12 and 24 hours after the onset of chest pain [23]. Weaker recommendations are given for PPCI 12-24 hours after symptom onset in the absence of ongoing ischemia [21]. PPCI is not applied to all AMI patients because of concurrent factors related to patient and/or medical institutional background [24]. In particular, older patients with AMI often have multiple comorbidities and physical disabilities [25,26] which might have negative effects on decisions regarding PPCI made by general or interventional cardiologists [24]. Other patient populations at risk for disparities include those with diabetes and those with chronic kidney disease [27]. Clinical variables such as higher age, female sex, and higher Killip class (The Killip classification was introduced for clinical assessment of patients with acute MI, and it stratifies individuals according to the severity of their post-MI HF [28]), and renal dysfunction, but not functional status on admission, were predictors of non-application of PPCI [24].
Regarding the above, the decision on how to treat STEMI patients is always difficult due to numerous influencing factors. There are several reasons and factors underlying the choice of reperfusion treatment, such as the Patient's age, gender, Killip class, underlying diseases, and late referral to the medical center due to lack of familiarity with the symptoms of myocardial infarction, etc. [24,25,27,29]. Some of these factors that influence treatment choices can be controlled by preventive nursing measures. For example, in late referral to the medical center, a policy should be adopted to provide the necessary information to the community by providing training courses to specific population groups on the symptoms of myocardial infarction and the need for prompt treatment. How to deal with a person with chest pain, avoiding wasting time, and quickly contacting the emergency room are the main pillars of treating this disease. If an emergency room is not available, the community should be aware of centers equipped with treatment facilities and get to these centers as soon as possible. These matters depend to a large extent on the education and awareness of the community, and increasing public awareness, whether through promotional displays and posters or through lectures and workshops, can be very effective in this regard. In Iran, no study was found that investigated the influencing factors in choosing the treatment of myocardial infarction. Assessing these factors can help overcome barriers to preferred STEMI treatment. In addition, by analyzing and comparing the side effects and outcomes of various treatment approaches, the effectiveness of thrombolytic therapy can be ensured to be a suitable alternative treatment to PPCI in specific circumstances.
Objectives
This study aimed to determine treatment selection factors and outcomes in acute cardiac infarction patients.
Methods
This cross-sectional and retrospective study examined the data of 252 myocardial infarction patients referred to Ayatollah Mousavi Hospital from April 2021 to March 2022 (Fig. 1).
Ayatollah Mousavi Hospital is a specialized center for heart services in Zanjan province. Code 247 is used for treating MI patients in the province. The telephone triage unit promptly responds to the patient's EMS call as per Code 247 policy. An electrocardiography (ECG) is taken immediately from the patient and sent to a specialist after the ambulance is dispatched. Code 247 is activated with an initial MI diagnosis, notifying the target hospital and the supervisor. Patients with ST-elevation MI are sent to the angiographic unit, whereas those with non-ST-elevation MI are referred to an emergency medicine specialist. However, STIM patients may not always be sent to the angiography department for various reasons.
Based on a study by Hanifi et al. [30], the minimum sample size of 196 people for sampling adequacy was estimated considering a standard deviation of 140 minutes for the time to treatment, a sampling error of 20 minutes, a power of 80%, and a confidence level of 95%. Convenience sampling was utilized in the present study. The medical records of all patients diagnosed with STEMI were thoroughly reviewed from April 1st, 2021 to March 31st, 2022. Out of the 340 patients diagnosed with STEMI, a total of 252 eligible patients were carefully chosen and their information was thoroughly analyzed. The medical records of patients with a diagnosis of STEMI (as determined by clinical symptoms, electrocardiogram changes, and elevated cardiac enzymes by the American College of Cardiology (ACC) and the American Heart Association (AHA) guidelines [31]) were selected for inclusion in the study. Study exclusion criteria were medical records of patients who had received thrombolytic therapy at another center before being referred to Ayatollah Mousavi Hospital and medical records with incomplete information.
The variables studied in this research were:
1. The possible determining factors for choosing the primary treatment intervention
2. Success or failure of treatment (Treatment success is determined by ST-Elevation removal of at least 50% in ECG or relief of chest pain within 90 minutes.)
3. Mechanical and electrical complications following treatment
4. Clinical outcomes (hospitalization cost, length of hospital stay, number of painkiller prescriptions),
5. One-year death rate and readmission due to heart problems within one year
The checklist used for data collection was prepared by reviewing past evidence and expert professors of the intensive care unit of the Zanjan School of Nursing and Midwifery opinions. The checklist was created by consulting trustworthy scientific literature [31-35]. Instrument validity was assessed using content validity. The designed instrument was presented to 10 experts (Professors and nurses with experience in the field of coronary care), and necessary changes were made according to their opinions. The reliability of the instrument was checked using inter-rater agreement. Both researchers completed the designed tool for ten patients to ensure reliability. The Kappa agreement coefficient between the two researchers was 95%.
Descriptive statistics were employed for data analysis, utilizing the mean and standard deviation for quantitative variables and frequency and percentage for qualitative variables. The normality of the data was assessed by analyzing the data's skewness and kurtosis. The Chi-square test/Fisher's exact test was utilized to assess the possible factors correlated with the selection of treatment intervention. Multiple logistic regression analysis was used to analyze the selection of primary intervention for reperfusion and identify associated predictors. Analysis of variance was utilized to assess and contrast clinical outcomes across diverse treatment groups. Furthermore, The Chi-square test/Fisher's exact test was utilized to compare the incidence of mechanical and electrical complications, readmission rates, and one-year mortality among the treatment groups for STEMI. Statistical analyses were conducted using SPSS version 22 software with a significance level set at 0.05.
|
340 STEMI patients were admitted to Ayatollah Mousavi Hospital in one year
|
|
88 patients were excluded from the study
|
|
Data from 252 patients was included in the study
|
|
Classifying patients into three groups according to primary intervention.
|
|
115 patients underwent PPCI
|
|
48 patients did not receive
treatment |
|
89 patients underwent thrombolytic therapy
|
|
Obtain patient demographic and clinical data.
Success or failure rate of primary treatment. Mechanical and electrical complications rate after primary treatment Death and readmission rate within a year Primary intervention selection factors |
Figure 1.
Study diagram
Results
Out of 340 patients with STEMI in this study, 88 were excluded due to receiving treatment elsewhere or incomplete medical records. The data of 252 patients with STEMI was finally analyzed. In the present study, the most common primary therapeutic intervention was PPCI (45.6 %). Thrombolytic therapy was the initial treatment for 35.3% of patients. Thrombolytic therapy was unsuccessful in 41.1% of patients and these patients underwent PCI Rescue. Only heparin and nitroglycerin were used for 19% of patients in the initial stage with no intervention.
Based on Table 1, the ANOVA test showed that there was a statistically significant difference in mean age between the treatment groups. In a pairwise comparison of groups, the no-intervention group had a significantly higher mean age than the thrombolytic therapy group (p=0.032) and the PPCI group (p=0.014). However, the mean age did not differ significantly between the two groups of thrombolytic therapy and PPCI (p>0.05). The gender distribution in various treatment groups showed significant differences (p=0.02). PPCI was the most common treatment for male patients. The average vital signs) include: systolic/diastolic blood pressure, heart rate, respiratory rate and Oxygen saturation (and Killip score did not show a statistically significant difference across various treatment groups (p>0.05). The time it took for the group with no intervention to reach the hospital differed significantly from the PPCI and thrombolytic therapy groups (p=0.0001). The time from hospital arrival to treatment initiation was significantly longer in the no-intervention group compared to the PPCI and thrombolytic therapy groups (p=0.0001). The PPCI group experienced a significantly longer delay between hospital arrival and treatment initiation compared to the thrombolytic therapy group (p=0.005). The groups showed significant differences in average pain levels before and after blood reperfusion, with the no-intervention group experiencing less pain before blood reperfusion than the PPCI and thrombolytic therapy group (p<0.001). The pain post-reperfusion was significantly lower in the PPCI and no intervention groups compared to the thrombolytic therapy group (p<0.001) (Table 1).
Table 1. Comparing Demographic and Clinical Characteristics of STEMI Patients Based on Treatment Selection
| p | No intervention | Thrombolytic therapy | PPCI | Quantitative variables |
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| 0.039* | 67.2 (11.2) | 62.6 (12.6) | 62.1 (11.6) | Age |
| 0.335* | 125.4 (23.4) | 132.5 (21.7) | 132.8 (35.2) | Systolic blood pressure(mmHg) |
| 1.92* | 76.2 (20.8) | 82.8 (13.1) | 80.7 (21.8) | Diastolic blood pressure(mmHg) |
| 0.146* | 80.0 (17.2) | 79 (17.8) | 78.3 (19.5) | Pulse rate(minutes) |
| 0.102* | 21.3 (6.3) | 19.4 (3.9) | 19.5 (5.8) | Respiratory rate (minutes) |
| 0.668* | 88.8 (14.1) | 90.4 (14.7) | 88.1 (21.3) | Oxygen saturation (SpO2) |
| 0.609* | 2.2 (1.2) | 2.0 (1.0) | 2.1 (1.0) | Killip calcification |
| <0.001* | 3.2 (3.0) | 9.3 (1.4) | 8.8 (2.1) | Pre-therapeutic pain level |
| <0.001* | 0 | 3.7 (3.3) | 1.7 (1.7) | Post-therapeutic pain level |
| <0.001* | 3252.6 (3985.0) | 315.5 (444.9) | 458.6 (796.3) | Pain-to-hospital arrival time (minutes) |
| <0.001* | 200.0 (216.1) | 44.7 (40.8) | 66.9(45.6) | Hospital arrival time for treatment (minutes) |
| p | No intervention | Thrombolytic therapy | PPCI | Qualitative variables |
| n (%) | n (%) | n (%) | ||
| 0.02** | 31 (64.6) | 68 (76.4) | 97 (84.3) | Male gender risk factor |
| 0.487** | 15 (31.2) | 20 (22.5) | 27 (23.5) | Diabetic |
| 0.287** | 27 (56.2) | 39 (43.8) | 50 (43.5) | Hypertension |
| 0.517** | 9 (18.7) | 11 (12.3) | 20 (17.4) | Hypercholesteremia |
| 0.03** | 15 (31.2) | 46 (51.7) | 42 (36.5) | Smoking |
| 0.98** | 9 (18.7) | 17 (19.1) | 21 (18.3) | Drug use |
| 0.29** | 17 (35.4) | 21 (23.6) | 29 (25.2) | Previous heart disease |
| 0.13** | 2 (4.2) | 0 | 4 (3.5) | History of stroke |
STEMI: ST Elevation Myocardial Infarction;
ANOVA: Analysis of variance; *ANOVA; ** chi-square teste
The availability of a 24/7 operational catheterization lab and an interventional cardiologist were factors influencing the selection of PPCI as the initial treatment (P=0.001). The non-intervention group had significantly higher rates of spontaneous reperfusion (p=0.001) (which manifested as resolution of the ST-segment elevation on ECG (transient STEMI) and/or normal coronary flow (Thrombolysis in Myocardial Infarction [TIMI] flow grade 3) in the infarct-related artery (IRA) at angiography before PCI), delayed diagnosis (p=0.032), and neglected MI (p=0.001). The patient's admission on a holiday and the attending physician's discretion were also significantly linked to the selection of thrombolytic treatment as the initial therapy (P=0.001). The choice of treatment did not show a significant relationship with hospital admission shift (p=0.323) or Killip score (p=0.315) (Table 2).
The Likelihood Ratio test in multiple regression analysis revealed that the availability of a 24.7 operational catheterization lab and the interventional cardiologist were predictors of the treatment selection. The selection of PPCI treatment has been predicted by the availability of an interventional cardiologist, with odds of 3.27 (OR =3.27, 95% CI: 7.93-93.67) (Table 3).
Table 4 shows that the success rate of PPCI was 87.2% and thrombolytic therapy was 58.9%. The success rate of PPCI treatment was significantly greater than that of thrombolytic therapy (p=0.01). Hematuria was the only mechanical complication related to the type of initial intervention in STEMI cases (p=0.002), with a higher incidence in the thrombolytic therapy group. Cardiac arrest was the only electrical complication related to the type of primary intervention (p=0.032), occurring more frequently in the PPCI group (Table 4).
ANOVA: Analysis of variance; *ANOVA; ** chi-square teste
The availability of a 24/7 operational catheterization lab and an interventional cardiologist were factors influencing the selection of PPCI as the initial treatment (P=0.001). The non-intervention group had significantly higher rates of spontaneous reperfusion (p=0.001) (which manifested as resolution of the ST-segment elevation on ECG (transient STEMI) and/or normal coronary flow (Thrombolysis in Myocardial Infarction [TIMI] flow grade 3) in the infarct-related artery (IRA) at angiography before PCI), delayed diagnosis (p=0.032), and neglected MI (p=0.001). The patient's admission on a holiday and the attending physician's discretion were also significantly linked to the selection of thrombolytic treatment as the initial therapy (P=0.001). The choice of treatment did not show a significant relationship with hospital admission shift (p=0.323) or Killip score (p=0.315) (Table 2).
The Likelihood Ratio test in multiple regression analysis revealed that the availability of a 24.7 operational catheterization lab and the interventional cardiologist were predictors of the treatment selection. The selection of PPCI treatment has been predicted by the availability of an interventional cardiologist, with odds of 3.27 (OR =3.27, 95% CI: 7.93-93.67) (Table 3).
Table 4 shows that the success rate of PPCI was 87.2% and thrombolytic therapy was 58.9%. The success rate of PPCI treatment was significantly greater than that of thrombolytic therapy (p=0.01). Hematuria was the only mechanical complication related to the type of initial intervention in STEMI cases (p=0.002), with a higher incidence in the thrombolytic therapy group. Cardiac arrest was the only electrical complication related to the type of primary intervention (p=0.032), occurring more frequently in the PPCI group (Table 4).
Table 2. Factors Related to Treatment Intervention Selection
* Fisher exact test; **Chi-square
Table 3. Predicting Treatment Decisions in Myocardial Infarction Patients (Reference Class: No Intervention)
PPCI: Primary Percutaneous Coronary Intervention
Table 4. Frequency (%) of Success and Complications (Mechanical and Electrical) after Therapeutic Intervention
| p | No intervention | Thrombolytic therapy | PPCI | Variable | |
| n (%) | n (%) | n (%) | |||
| 0.001* | 44 (91.7) | 72 (80.9) | 113 (98.3) | Yes | The activity level of the catheterization lab |
| 4 (8.3) | 17 (19.1) | 2 (1.7) | No | ||
| 0.001* | 18 (37.5) | 24 (27.0) | 111 (96.5) | Yes | availability of an interventional cardiologist |
| 30 (62.5) | 65 (73.0) | 4 (3.5) | No | ||
| 0.001* | 4 (8.3) | 0 | 0 | Yes | Early spontaneous reperfusion |
| 44 (91.7) | 89 (100) | 115 (100) | No | ||
| 0.032* | 3 (6.2) | 0 | 2 (1.7) | Yes | Failure to timely diagnose. |
| 45 (93.8) | 89 (100) | 113 (98.3) | No | ||
| 0.001* | 32 (66.7) | 0 | 2 (1.7) | Yes | Neglected Myocardial infarction |
| 16 (33.3) | 89 (100) | 113 (98.3) | No | ||
| 0.001* | 3 (6.2) | 14 (15.7) | 0 | Yes | The interventional cardiologist will decide on the treatment method without specifying the reason |
| 45 (93.8) | 75 (84.3) | 115 (100) | No | ||
| 0.323** | 9 (18.7) | 21 (23.6) | 36 (31.3) | Morning | Hospital admission shift |
| 20 (41.7) | 27 (30.3) | 35 (30.4) | Evening | ||
| 19 (39.6 | 41 (46.1) | 44 (38.2) | Night | ||
| 0.001** | 12 (25) | 40 (44.9) | 25 (21.7) | Yes | Patient admission in Holliday |
| 36 (75) | 49 (55.1) | 90 (78.2) | No | ||
| 0.315** | 20 (41.7) | 33 (37.1) | 41 (35.6) | I | Killip classification |
| 10 (20.8) | 30 (33.7) | 31 (26.9) | II | ||
| 8 (16.7) | 18 (20.22) | 29 (25.2) | III | ||
| 10 (20.8) | 8 (9.0) | 14 (12.2) | IV | ||
| 0.001* | 5 (10.4) | 88 (98.9) | 115 (100) | Yes | Patient’s consent for treatment |
| 3 (6.2) | 0 | 0 | No | ||
| 1 (2.1) | 1 (1.1) | 0 | Delayed consent | ||
| 39 (81.3) | 0 | 0 | |||
| Consent not necessary |
* Fisher exact test; **Chi-square
Table 3. Predicting Treatment Decisions in Myocardial Infarction Patients (Reference Class: No Intervention)
| Multiple regression analysis | Independent variable | ||||
| 95% Confidence Interval Lower Bound-Upper Bound |
Exp (B) | p | B | ||
| 0.09-10.03 | 0.95 | 0.968 | -0.05 | PPCI | the activity level of the catheterization lab |
| 0.01-0.74 | 0.11 | 0.023 | -2.18 | Thrombolytic therapy | |
| 7.93-93.67 | 26.32 | 0.001 | 3.27 | PPCI | availability of an interventional cardiologist |
| 0.82-10.94 | 2.98 | 0.098 | 1.09 | ||
| Thrombolytic therapy |
PPCI: Primary Percutaneous Coronary Intervention
Table 4. Frequency (%) of Success and Complications (Mechanical and Electrical) after Therapeutic Intervention
| p | No intervention | Thrombolytic therapy | PPCI | Variable |
| n (%) | n (%) | n (%) | ||
| 0.01** | - | (58.9) 53 | 102 (87.2) | Therapeutic success |
| 0.194** | (20.8) 10 | (10.1) 9 | 14 (12.2) | Cardiogenic shock |
| 0.686** | (33.3) 16 | (32.6) 29 | 44 (38.3) | Pulmonary edema |
| 0.174** | (75.0) 36 | (82.0) 73 | 100 (86.9) | Heart failure |
| 0.582* | (4.2) 2 | (2.2) 2 | 6 (5.2) | Recurrent myocardial infarction (re-MI) |
| 0.752* | (4.2) 2 | (6.7) 6 | 5 (4.3) | Gastrointestinal bleeding. |
| 0.655* | (6.2) 3 | (3.4) 3 | 7 (6.1) | Blood sputum |
| 0.002* | 0 | ((16.8 15 | 8 (6.9) | Hematuria |
| 0.667* | (4.2) 2 | 0 | 4 (3.5) | Stroke |
| 0.032** | (25.0) 12 | (9.0) 8 | 15 (13.0) | Cardiac arrest |
| 0.556** | (37.5) 18 | (40.4) 36 | 38 (33.0) | Premature ventricular contractions |
| 0.436** | (22.9) 11 | (16.8) 15 | 17 (14.8) | Ventricular tachycardia |
| 0.671* | (8.3) 4 | (6.7) 6 | 12 (10.4) | Ventricular Fibrillation |
| 1.0* | (2.1) 1 | (2.2)2 | 2 (1.7) | Paroxysmal supraventricular tachycardia |
| 0.288** | (12.5) 6 | (11.2) 10 | 7 (6.1) | Atrial fibrillation |
| 0.345** | (35.4) 17 | (38.2) 24 | 33 (28.7) | Bradycardia |
| 0.763** | (41.7) 20 | (36) 32 | 46 (40.0) | Tachycardia |
| 1.0* | 0 | (1.1) 1 | 2 (1.7) | First-degree atrioventricular (AV) block |
| 0.351* | 0 | (1.1) 1 | 4 (3.5) | Second-Degree Atrioventricular Block |
| 0.667* | (6.2) 3 | (3.4) 3 | 5 (4.3) |
| Complete Heart Block |
* Fishers exact test; **Chi-square
Discussion
Studies have proven the superiority of PPCI over thrombolytic therapy for STEMI patients hospitalized within the golden period [14,16,17, 36], but this method requires special facilities, and the number of centers providing this technique are limited [20]. Achievement of reperfusion via PPCI with an experienced operator in the "golden time" in many countries is a problematic issue [35]. Parts of Iran face limitations that make it challenging to achieve a 24.7 environment for PPCI. The patient's condition may prevent PPCI intervention. The purpose of this study is twofold: first, to identify factors influencing the choice of myocardial infarction treatment that can help remove barriers to PPCI. Second, to compare myocardial infarction treatment methods so that, in the absence of differences in treatment outcomes, thrombolytic therapy can be an alternative to PPCI in certain uncorrectable conditions. Therefore, this study designed to determine treatment selection factors and outcomes in acute cardiac infarction patients.
The no-intervention group had a higher average age than the thrombolytic therapy and PPCI group in the current study. Young patients often underwent PPCI or thrombolytic therapy for timely referral to medical centers. late presentation to the hospital of neglected MI in older patients, who did not receive primary intervention, resulted in missed opportunities for blood reperfusion. Young patients were more familiar with the symptoms of myocardial infarction and the complications of not treating it promptly than older patients, so they were referred to medical centers more quickly and had a greater chance of receiving reperfusion therapy. There was no statistical difference in the average age of the PPCI and thrombolytic therapy groups in some studies [34,37-39]. In a study, the thrombolytic therapy group had a lower average age compared to the PPCI group [35]. There was no study that compared the average age in the no-intervention group with the thrombolytic therapy and PPCI group.
In the present study, male patients mostly received PPCI, whereas, in Soleimani et al.'s study, men were mostly treated with thrombolytic therapy [35]. Treatment selection based on gender had no significant difference in other studies [34, 38,40]. Thrombolytic therapy was administered to the majority of smoking patients in the study, in line with Soleimani et al.'s findings [35]. Similar to previous studies, the finding of the present study revealed no significant difference in mean vital signs and Killip score within the selected treatment group [17,20,31,40].
Patients were primarily treated with PPCI based on the availability of a 24/7 operational catheterization lab and an interventional cardiologist and written informed consent patient. In the case of spontaneous reperfusion, failure to diagnose STEMI on time, or Neglected MI, patients might not receive immediate intervention and instead were given routine medications like heparin and nitroglycerin. Thrombolytic therapy was the primary treatment for patients admitted on holidays. The Likelihood Ratio test in regression analysis demonstrated that catheterization lab activity and interventional cardiologist availability predicted treatment selection. the present study showed that younger individuals (patients aged 32-52 compared to patients over 73) were more likely to be considered for PPCI, although Killip's classification did not play a role in the decision of primary treatment. Aging, chronic renal failure, and higher Killip classification were negatively correlated with PPCI and thrombolytic therapy in some studies [24,41].
Similar to Pu et al.'s study [17], in the present study among the mechanical complications of STEMI only the incidence of hematuria was significantly associated with the type of initial intervention, so the incidence of this complication was higher in the thrombolytic group. In line with prior studies, there was no statistically significant difference in other mechanical complications between the treatment groups [34,39,40].
Khan et al.'s study found that the thrombolytic therapy group had a significantly higher rate of stroke, recurrent myocardial infarction, and heart failure compared to the PPCI group [42], which goes against the results of the present study. The potential reason for the difference between the results of the current study and the above-mentioned research could be the effect of age on patient outcomes, since older patients may have more underlying diseases, which in turn can increase complications rate; accordingly, studies including patients within different age groups could have different complications rates following PCI or thrombolytic therapy. In Khan et al.'s study, the mean age of the thrombolytic group was higher than the PPCI group, which could be responsible for the higher incidence of complications in this group. Similar to a previous study, the treatment groups did not show a significant difference in the electrical complications caused by STEMI [35]. Only the incidence of cardiac arrest was higher in the PPCI group than in the other two groups.
The duration of hospitalization was much longer for the group that did not receive initial intervention, in contrast to both the PPCI group and the thrombolytic therapy group. However, there was no difference in the length of hospital stay between the thrombolytic therapy and PPCI groups. Therefore, it can be concluded that patients who did not receive initial intervention had a longer hospital stay. According to Kazemi et al, the thrombolytic therapy and PPCI groups had the same hospital stay duration [40]. The data suggests that the group receiving no intervention had a relatively higher mortality rate after one year when compared to the PPCI and thrombolytic treatment groups. Nevertheless, this distinction did not show statistical significance, which is consistent with the results of previous research [17,31,34, 35,37,39].
A notable strength of this study was its analysis of treatment factors and outcomes across three groups: PPCI, thrombolytic therapy, and no intervention. The study's retrospective approach restricts access to accurate information, highlighting the importance of future prospective studies.
Conclusion
Addressing barriers is crucial to promote timely PPCI over thrombolytic therapy. In countries where achieving the "golden time" for PPCI treatment is difficult, thrombolytic therapy followed by rescue PCI is a highly effective alternative. The study revealed that there were no significant differences in complications, clinical outcomes, mortality, and rehospitalization between patients who underwent PPCI and those treated with thrombolytic therapy. Thus, thrombolytic therapy remains a viable alternative when timely PPCI treatment cannot be achieved. Patients who couldn't receive PPCI for any reason might be stressed about not receiving their preferred treatment. Thrombolytic therapy's effectiveness can be reinforced by the findings of this study.
Ethical Consideration
The ethics committee of Zanjan University of Medical Sciences granted permission for the research, registered as IR.ZUMS.REC.1400.496. By presenting a written letter of introduction from the Research Vice-Chancellor of Zanjan University of Medical Sciences, the researcher was introduced to the directorate of Ayatollah Mousavi Hospital. Before conducting the research, the officials were informed about its purpose and nature to secure their cooperation. Officials were assured that patient information would be confidential, and when reviewing patient records, they would omit patient characteristics and identity details.
Acknowledgments
The authors appreciate the support of the staff of Ayatollah Mousavi Hospital.
Conflict of interest
The authors declares they have no conflict of interest.
Funding
The Research and Technology Vice-Chancellor of Zanjan University of Medical Sciences has funded this project.
Authors' contributions
Hanifi N., Gholamian E., and Shiri Ghidari P. were responsible for the study design. Gholamian E. gathered the data. All authors were responsible for statistical analysis and interpretation of the data, drafting of the manuscript, and critical revision of the manuscript.
Artificial Intelligence Utilization
The authors did not use any Artificial Intelligence (AI) tools or technologies during the preparation of this manuscript.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to privacy restrictions but are available from the corresponding author upon reasonable request.
Type of Study: Orginal research |
Subject:
Nursing
References
1. 1. Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde-Price C, et al. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. Journal of the American College of Cardiology. 2014;64(4):337-45. [https://doi.org/10.1016/j.jacc.2014.04.054] [PMID]
2. Sharif Nia H, Chehrzad MM, Froelicher ES, Pahlevan Sharif S, Yaghoobzadeh A, Jafari A, et al. Weather fluctuations: predictive factors in the prevalence of acute coronary syndrome. Health Promotion Perspectives. 2019;9(2):123-30. [https://doi.org/10.15171/hpp.2019.17] [PMID]
3. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019. Journal of the American College of Cardiology. 2020;76(25):2982-3021. [https://doi.org/10.1016/j.jacc.2020.11.010] [PMID]
4. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. European Heart Journal. 2018;39(2):119-77. [https://doi.org/10.1093/eurheartj/ehx393] [PMID]
5. Bhatnagar P, Wickramasinghe K, Williams J, Rayner M, Townsend N. The epidemiology of cardiovascular disease in the UK 2014. British Medical Journal. 2015;101(15):1182-9. [https://doi.org/10.1136/heartjnl-2015-307516] [PMID]
6. Jayaraj JC, Davatyan K, Subramanian S, Priya J. Epidemiology of myocardial infarction. In: Myocardial Infarction [Internet]. London (UK): IntechOpen; 2019. p. 9-19. [https://doi.org/10.5772/intechopen.74768] [PMID]
7. Roger VL. Epidemiology of myocardial infarction. Medical Clinics of North America. 2007;91(4):537-52. [https://doi.org/10.1016/j.mcna.2007.03.007] [PMID]
8. Ahmadi A, Sajjadi H, Etemad K, Khaledifar A, Mobasherii M. Epidemiological characteristics and determinants of mortality in acute coronary syndrome in Iran. International Journal of Cardiovascular Practice. 2015;25(124):1-9. [http://jmums.mazums.ac.ir/article-1-5688-fa.html]
9. Sharif Nia H, Gorgulu O, Pahlevan Sharif S, Froelicher ES, Haghdoost AA, Golshani S, et al. Prevalence of acute myocardial infarction and changing meteorological conditions in Iran: fuzzy clustering approach. Iranian Journal of Public Health. 2020;49(5):923-30. [https://doi.org/10.18502/ijph.v49i5.3210] [PMID]
10. Mohammadpour RA, Khanali F, Yazdani J, Mahmoodi M, Khosravi A. Estimating potential gain in life expectancy by eliminating causes of death in Iran, 2010. Journal of Mazandaran University of Medical Sciences. 2014;24(112):89-95. [http://jmums.mazums.ac.ir/article-1-2693-en.html]
11. Tamis-Holland JE, O'Gara PT. Highlights from the 2013 ACCF/AHA Guidelines for the management of ST-elevation myocardial infarction and beyond. Clinical Cardiology. 2014;37(4):252-9. [https://doi.org/10.1002/clc.22258] [PMID]
12. Theodoridis PG, Davos CH, Dodos I, Iatrou N, Potouridis A, Pappas GM, et al. Thrombolysis in acute lower limb ischemia: review of the current literature. Annals of Vascular Surgery. 2018;52:255-62. [https://doi.org/10.1016/j.avsg.2018.02.030] [PMID]
13. Daei M, Karimi Rad M, Khalaja M. Reasons for not receiving thrombolytic therapy in patients with acute myocardial infarction admitted to Bu-Ali Sina Hospital in Qazvin (2013-14). Journal of Qazvin University of Medical Sciences. 2017;21(1):79-83. [https://core.ac.uk/reader/95377030]
14. Fazel R, Joseph TI, Sankardas MA, Pinto DS, Yeh RW, Kumbhani DJ, et al. Comparison of reperfusion strategies for ST-segment-elevation myocardial infarction: a multivariate network meta-analysis. Journal of the American Heart Association. 2020;9(12):e015186. [https://doi.org/10.1161/JAHA.119.015186] [PMID]
15. Lindsey ML, Brás LEdC, DeLeon-Pennell KY, Frangogiannis NG, Halade GV, O'Meara CC, et al. Reperfused vs. nonreperfused myocardial infarction: when to use which model. American Journal of Physiology - Heart and Circulatory Physiology. 2021;321(1):H208-13. [https://doi.org/10.1152/ajpheart.00234.2021] [PMID]
16. Martínez-Sánchez C, Arias-Mendoza A, González-Pacheco H, Araiza-Garaygordobil D, Marroquín-Donday LA, Padilla-Ibarra J, et al. Reperfusion therapy of myocardial infarction in Mexico: a challenge for modern cardiology. Archivos de Cardiologia de Mexico. 2017;87(2):144-50. [https://doi.org/10.1016/j.acmx.2016.12.007] [PMID]
17. Pu J, Ding S, Ge H, Han Y, Guo J, Lin R, et al. Efficacy and safety of a pharmaco-invasive strategy with half-dose alteplase versus primary angioplasty in ST-segment-elevation myocardial infarction. Circulation Journal. 2017;136(16):1462-73. [https://doi.org/10.1161/CIRCULATIONAHA.117.030582] [PMID]
18. Llevadot J, Giugliano RP, Antman EM. Bolus fibrinolytic therapy in acute myocardial infarction. Journal of the American Medical Association. 2001;286(4):442-9. [https://doi.org/10.1001/jama.286.4.442] [PMID]
19. Zhao X, Yang X, Gao C, Chu Y, Yang L, Tian L, et al. Improved survival of patients with ST-segment elevation myocardial infarction 3-6 hours after symptom onset is associated with inter-hospital transfer for primary percutaneous coronary intervention (PCI) at a large regional STEMI program vs. in-hospital thrombolysis in a community hospital. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research. 2017;23:1055-63. [https://doi.org/10.12659/MSM.902466] [PMID]
20. Izadpanah P, Falahati F, Mokhtari AM, Hosseinpour F, Faham B, Sheidaee R, et al. The survival rate of patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention and thrombolysis. Clinical Epidemiology and Global Health. 2020;8(3):770-4. [https://doi.org/10.1016/j.cegh.2020.01.017]
21. Frampton J, Devries JT, Welch TD, Gersh BJ. Modern management of ST-segment elevation myocardial infarction. Current Problems in Cardiology. 2020;45(3):100393. [https://doi.org/10.1016/j.cpcardiol.2018.08.005] [PMID]
22. Kastrati A, Coughlan J, Ndrepepa G. Primary PCI, late presenting STEMI, and the limits of time. Journal of the American College of Cardiology. 2021;78(13):1306-8. [https://doi.org/10.1016/j.jacc.2021.08.001] [PMID]
23. Late Study Group. Late assessment of thrombolytic efficacy (LATE) study with alteplase 6-24 hours after onset of acute myocardial infarction. The Lancet. 1993;342(8874):759-66. [https://doi.org/10.1016/0140-6736(93)91538-W]
24. Uemura S, Okamoto H, Nakai M, Nishimura K, Miyamoto Y, Yasuda S, et al. Primary percutaneous coronary intervention in elderly patients with acute myocardial infarction: an analysis from a Japanese nationwide claim-based database. Circulation Journal. 2019;83(6):1229-38. [https://doi.org/10.1253/circj.CJ-19-0004] [PMID]
25. Avezum A, Makdisse M, Spencer F, Gore JM, Fox KA, Montalescot G, et al. Impact of age on management and outcome of acute coronary syndrome: observations from the Global Registry of Acute Coronary Events (GRACE). American Heart Journal. 2005;149(1):67-73. [https://doi.org/10.1016/j.ahj.2004.06.003] [PMID]
26. Skolnick AH, Alexander KP, Chen AY, Roe MT, Pollack CV Jr, Ohman EM, et al. Characteristics, management, and outcomes of 5,557 patients aged ≥90 years with acute coronary syndromes: results from the CRUSADE initiative. Journal of the American College of Cardiology. 2007;49(17):1790-7. [https://doi.org/10.1016/j.jacc.2007.01.066] [PMID]
27. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, De Lemos JA, et al. 2013 ACCF/AHA Guideline for the management of ST-elevation myocardial infarction: executive summary. Circulation Journal. 2013;127(4):529-55. [https://doi.org/10.1161/CIR.0b013e3182742c84] [PMID]
28. Hashmi KA, Adnan F, Ahmed O, Yaqeen SR, Ali J, Irfan M, et al. Risk assessment of patients after ST-segment elevation myocardial infarction by Killip classification: an institutional experience. Cureus. 2020;12(12):e12209. [https://doi.org/10.7759/cureus.12209]
29. Frampton J, Devries JT, Welch TD, Gersh BJ. Modern management of ST-segment elevation myocardial infarction. Current Problems in Cardiology. 2020;45(3):100393. [https://doi.org/10.1016/j.cpcardiol.2018.08.005] [PMID]
30. Hanifi N, Rezaee E, Rohani M. Time-to-treatment and its association with complications and mortality rate in patients with acute myocardial infarction: a prospective cohort study. Journal of Emergency Nursing. 2021;47(2):288-98.e4. [https://doi.org/10.1016/j.jen.2020.05.013] [PMID]
31. Alimohammadzadeh K, Sadeghi R, Maher A, Kazemi MK. Short-term cost-effectiveness of reteplase versus primary percutaneous coronary intervention in patients with acute STEMI: a tertiary hospital in Iran. International Journal of Cardiovascular Practice. 2017;2(3):65-9. [https://doi.org/10.21859/ijcp-020305]
32. Daei M, Karimi Rad M, Khalaja M. Reasons for not receiving thrombolytic therapy in patients with acute myocardial infarction admitted to Bu-Ali Sina Hospital in Qazvin (2013-14). Journal of Qazvin University of Medical Sciences. 2017;21(1):79-83. [https://core.ac.uk/reader/95377030]
33. Falsoleiman H, Fatehi G, Dehghani M, Shakeri M, Bayani B, Ahmadi M, et al. Clinical outcome and survival between primary percutaneous coronary intervention versus fibrinolysis in patients older than 60 years with acute myocardial infarction. Heart Views. 2012;13(4):129-31. [https://doi.org/10.4103/1995-705X.105728] [PMID]
34. Kocayigit I, Yaylaci S, Osken A, Aydın E, Sahinkus S, Can Y, et al. Comparison of effects of thrombolytic therapy and primary percutaneous coronary intervention in elderly patients with acute ST-segment elevation myocardial infarction on in-hospital, six-month, and one-year mortality. Archives of Medical Sciences - Atherosclerotic Diseases. 2019;4:e82-8. [https://doi.org/10.5114/amsad.2019.85378] [PMID]
35. Soleimani M, Soleimani A, Roohafza H, Sarrafzadegan N, Taheri M, Yadegarfar G, et al. Comparison of procedural and clinical outcomes of thrombolytic-facilitated and primary percutaneous coronary intervention in patients with acute ST-elevation myocardial infarction (STEMI): findings from the PROVE/ACS study. ARYA Atherosclerosis. 2020;16(3):123-9. [https://doi.org/10.22122/arya.v16i3.1869]
36. Joy ER, Kurian J, Gale CP. Comparative effectiveness of primary PCI versus fibrinolytic therapy for ST-elevation myocardial infarction: a review of the literature. Journal of Comparative Effectiveness Research. 2016;5(2):217-26. [https://doi.org/10.2217/cer-2015-0011] [PMID]
37. Arnesen JS, Strøm KH, Bønaa KH, Wiseth R. Treatment of ST-elevation myocardial infarction - an observational study. Tidsskrift for den Norske Laegeforening: Tidsskrift for Praktisk Medicin, Ny Raekke. 2019;139(17):65-9. [https://doi.org/10.4045/tidsskr.18.0928]
38. Asadpour Piranfar M, Jafari Fesharaki M, Taati R. Comparison of the 3-month outcome between primary PCI and thrombolytic therapy concerning the left ventricular ejection fraction of STEMI patients at 90-minute intervals. Iranian Heart Journal. 2021;22(4):45-53. [https://journal.iha.org.ir/article_137647.html]
39. Zubaid M, Khraishah H, Alahmad B, Rashed W, Ridha M, Alenezi F, et al. Efficacy and safety of a pharmacoinvasive strategy compared to primary percutaneous coronary intervention in the management of ST-segment elevation myocardial infarction: a prospective country-wide registry. Annals of Global Health. 2020;86(1):1-8. [https://doi.org/10.5334/aogh.2632] [PMID]
40. Kazemi MK, Alimohammadzadeh K, Maher A. Short- and long-term follow-up in elderly patients with ST-elevation myocardial infarction receiving primary angioplasty or thrombolytic therapy. International Journal of Cardiovascular Practice. 2019;4(1):10-5. [https://doi.org/10.21859/ijcp-403]
41. Turk J, Fourny M, Yayehd K, Picard N, Ageron FX, Boussat B, et al. Age-related differences in reperfusion therapy and outcomes for ST-segment elevation myocardial infarction. Journal of the American Geriatrics Society. 2018;66(7):1325-31. [https://doi.org/10.1111/jgs.15383] [PMID]
42. Khan S, Islam SU, Samin A, Yousaf H, Ali U, Shaheen Z, et al. Difference in outcomes in patients with ST-elevation myocardial infarction treated with thrombolysis versus primary percutaneous coronary intervention. Pakistan Armed Forces Medical Journal. 2021;71(Suppl-2):S384-8. [https://pafmj.org/PAFMJ/article/view/7798]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |