
Preventive Care in Nursing and Midwifery Journal

Volume 15, Issue 3 (10-2025)
Prev Care Nurs Midwifery J 2025, 15(3): 61-70 |
Back to browse issues page
Ethics code: مروری
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shirozhan S, Shoja M, Metanat F, Motie M. Functional models in rehabilitation nursing care: A scoping review. Prev Care Nurs Midwifery J 2025; 15 (3) :61-70
URL: http://nmcjournal.zums.ac.ir/article-1-947-en.html
URL: http://nmcjournal.zums.ac.ir/article-1-947-en.html
Student Research Committee, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran , mahdiehmotie71@gmail.com
Full-Text [PDF 776 kb]
(162 Downloads)
| Abstract (HTML) (751 Views)
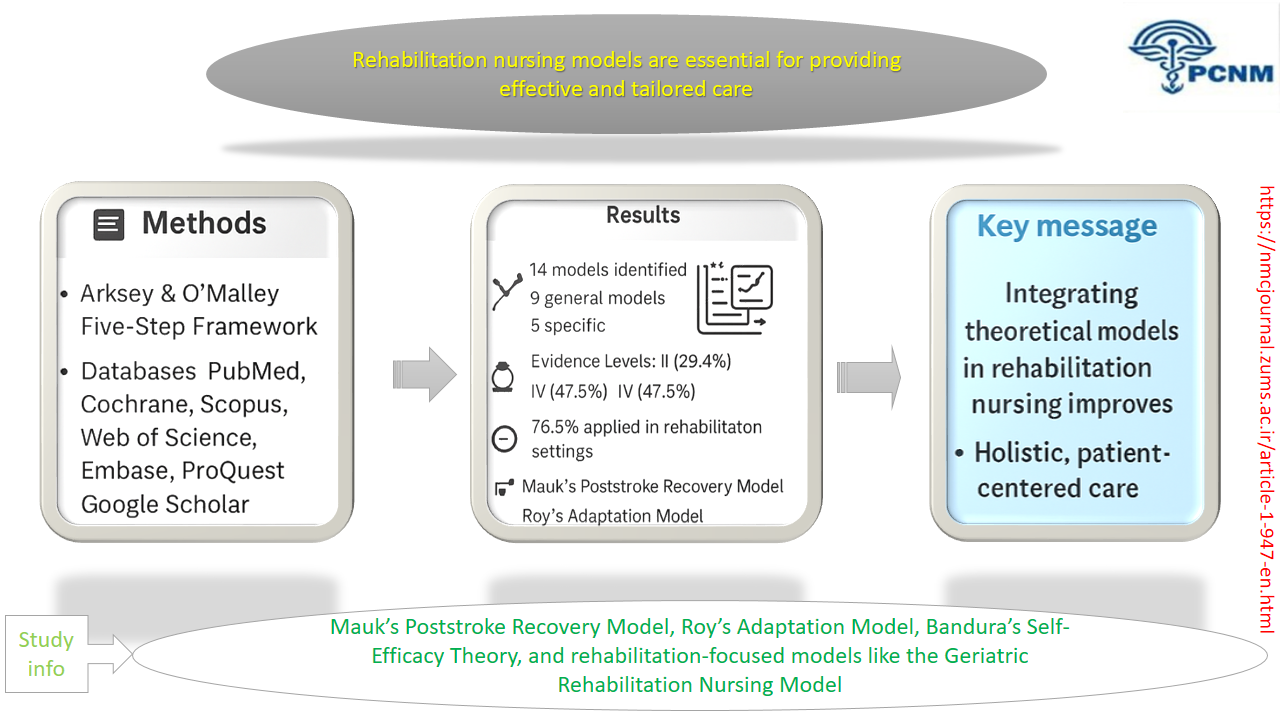
Table 2. Inclusion and Exclusion Criteria Based on the PICOS Framework
Study Selection
In the initial search, a total of 671 articles were identified. The selection process was conducted in two stages by two independent reviewers. In the first stage, titles and abstracts were screened to remove irrelevant studies, such as those that did not address nursing models or were unrelated to rehabilitation nursing. In the second stage, the full texts of 38 potentially relevant articles were reviewed in detail. Studies were excluded if they did not explicitly mention a nursing model, provided insufficient data about the model’s structure, or lacked clear methodological descriptions. Finally, 17 articles met the inclusion criteria and were included in the final analysis (Figure 1).
Data Extraction
A structured table was developed that included key information from each study, such as the purpose, year, type of study, theoretical or conceptual model used, and main findings. Additional columns were added for study setting, participants, country, and data collection methods. This comprehensive approach allowed for the identification of common themes, gaps, and trends.
Figure 1. PRISMA Flow Chart
Quality Appraisal
The methodological quality of the included studies was assessed using standardized appraisal tools appropriate for each study design. Randomized Controlled Trials (RCTs) were evaluated using the Cochrane Risk of Bias tool (RoB 2); qualitative studies were appraised using the CASP checklist; and case reports or series were assessed with the JBI Critical Appraisal Checklist.
Each study was independently reviewed by two researchers, and discrepancies were resolved through discussion and consensus.
While no studies were excluded solely based on quality, this appraisal informed the interpretation and synthesis of findings, highlighting methodological strengths and limitations.
Data Synthesis
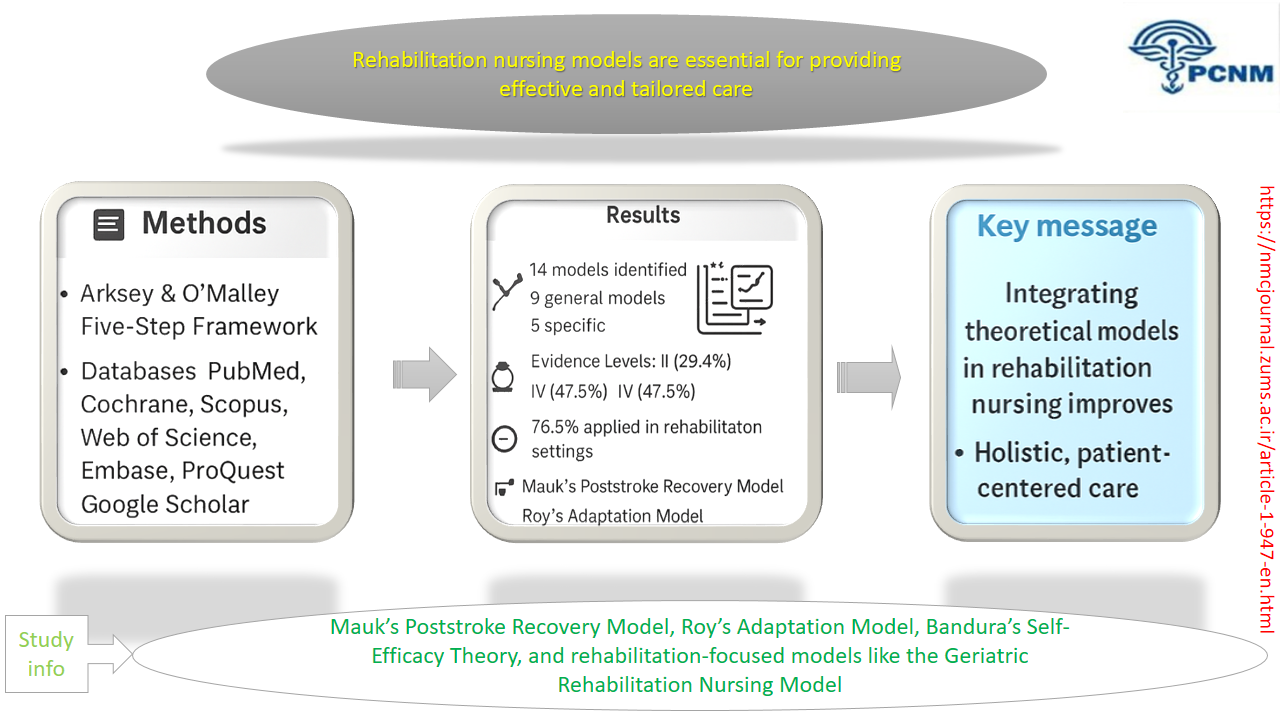
A total of fourteen models related to rehabilitation nursing were identified and categorized into two main groups: general models and specific models.
General models were adapted from broader nursing or healthcare frameworks, while specific models were designed explicitly for rehabilitation nursing. This categorization clarified the theoretical diversity and evolution of conceptual approaches within the field.
Results
From the articles reviewed, a total of 17 studies were selected for the final analysis. Among these, five articles (29.4%) were published within the last five years [14–18], all in international journals, with seven articles (41.1%) specifically published in rehabilitation journals [7, 19–23].
In terms of levels of evidence, eight articles (47.5%) provided level IV evidence [7, 16, 17, 19, 22–25], while five articles (29.4%) provided level II evidence [14, 15, 20, 21, 26] (Table 3).
In thirteen articles (76.47%), the models were directly applied to patients with conditions requiring rehabilitation, such as heart attacks [17, 18, 27, 28], cerebrovascular accidents (CVAs) [14, 15, 20–23], spinal cord injuries [25], burns [26], and pulmonary disorders [16]. Additionally, three articles (17.64%) discussed the development of new models. A total of fourteen models were identified and categorized into general and specific models. Of these, nine originated from the field of general nursing, while five were specific to rehabilitation nursing.
Table 3. Specifications of Selected Studies
From the nursing field, four models were foundational nursing theories:
Evidence levels varied across the reviewed studies, with nearly half providing level IV evidence and fewer offering higher-level (level II) studies. This underscores the need for more rigorous research to validate the effectiveness of rehabilitation nursing models and their impact on measurable patient outcomes. Moreover, the findings reveal persistent gaps such as fragmented information, limited theoretical integration, and a notable theory–practice gap in rehabilitation nursing [5, 8, 14].
Many existing models remain highly specialized, which limits their broader applicability and scalability. Furthermore, the lack of standardized evaluation tools and insufficient training on theory-based practice among nurses contribute to the underutilization of these models in real-world clinical environments [9, 10].
Overall, the findings indicate that rehabilitation nursing relies on a combination of general and specific models to guide practice. Strengthening the evidence base, enhancing methodological rigor, and developing flexible, context-specific models are essential steps to improve theoretical integration, guide clinical decision-making, and advance patient-centered rehabilitation care. Future research should aim to evaluate these models in diverse cultural and clinical contexts, explore their effectiveness in multidisciplinary settings, and identify strategies to bridge the gap between theory and practice
Conclusion
This review highlights that rehabilitation nursing models are essential for improving care quality and patient outcomes by addressing patients’ physical, psychological, and social needs. General models, such as Roy’s Adaptation Model and Orem’s Self-Care Model, demonstrate high adaptability across diverse patient populations, while specific models, including the Mauk Model for Poststroke Recovery and the Geriatric Rehabilitation Nursing Model, provide targeted frameworks for specialized rehabilitation care.
Despite their demonstrated benefits, many models remain underutilized in practice, with limited high-level evidence and inconsistent integration into clinical routines. To advance rehabilitation nursing, future research should focus on developing context-specific models for various patient groups, exploring strategies to bridge the theory–practice gap, integrating digital tools and tele-rehabilitation for enhanced self-management, and evaluating barriers and facilitators to implementation in real-world clinical settings.
Addressing these priorities can enhance evidence-based, patient-centered care, strengthen interdisciplinary collaboration, and improve functional and quality-of-life outcomes for patients with complex rehabilitation needs.
Ethical Considerations
This study was a scoping review of previously published articles and did not involve direct participation of human subjects. Therefore, ethical approval and informed consent were not required. All included studies were properly cited to acknowledge the original authors and their work.
Acknowledgments
The authors would like to thank the Department of Nursing at the University of Social Welfare and Rehabilitation Sciences for their continuous guidance and academic support.
Conflict of Interest
The authors declare that there are no conflicts of interest related to this study.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors’ Contributions
Shirozhan Sh. and Shoja M. contributed to the conceptualization and design of the study.
Metanat F. and Motie M. were responsible for data collection, analysis, and interpretation.
Motie M. led the drafting and critical revision of the manuscript.
All authors reviewed and approved the final version of the manuscript and agreed to be accountable for all aspects of the work.
Artificial Intelligence Utilization for Article Writing
No artificial intelligence tools were used in the writing, analysis, or preparation of this manuscript. All content and decisions were solely performed by the authors.
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary materials.
The data supporting the findings of this study are available from the corresponding author upon reasonable
Knowledge Translation Statement
Audience: Rehabilitation nurse managers, educators, curriculum developers, and healthcare administrators
A scoping review synthesizes and categorizes the diverse functional models guiding rehabilitation nursing, such as the Self-Care Model and the King's Theory of Goal Attainment. This synthesized map of the conceptual landscape serves as a foundational resource for educators to structure curricula and for managers to select and implement evidence-based models that systematically enhance patient outcomes and professional practice in rehabilitation settings.
Audience: Rehabilitation nurse managers, educators, curriculum developers, and healthcare administrators
A scoping review synthesizes and categorizes the diverse functional models guiding rehabilitation nursing, such as the Self-Care Model and the King's Theory of Goal Attainment. This synthesized map of the conceptual landscape serves as a foundational resource for educators to structure curricula and for managers to select and implement evidence-based models that systematically enhance patient outcomes and professional practice in rehabilitation settings.
Full-Text: (31 Views)
Introduction
The nursing profession encompasses numerous theories developed by nursing theorists or adapted from related fields, which represent a significant aspect of the discipline [1, 2]. These theories are utilized by nurses across various domains, including clinical practice, research, education, and nursing management, thereby enhancing the overall quality of the nursing profession [1, 3, 4]. Evidence indicates that nurses who provide theory-based care achieve better clinical outcomes compared to those delivering traditional care, particularly in areas such as self-efficacy, patient self-care, and overall quality of life [3, 5]. Furthermore, these theories not only shape nurses’ performance but also contribute to their job satisfaction [3, 5, 6].
In complex specialties such as rehabilitation nursing, the diverse and specific needs of patients necessitate accurate identification of their requirements and the provision of comprehensive care [7, 8]. It is essential to recognize that nursing theories exist at various levels of abstraction; some highly abstract theories may restrict their practical application in nursing care. Conversely, theories that are more concrete and specific are better suited for direct nursing practice [1, 6]. Additionally, aligning nursing theories and models with fundamental nursing principles, such as those emphasized in rehabilitation nursing, enhances their clinical utility.
Despite the demonstrated positive effects of theory-based care on clinical outcomes [2, 9, 10], the application of these theories in clinical nursing remains limited, and many nurses exhibit reluctance to adopt them. This reluctance may stem from a lack of familiarity with nursing theories and models among clinical nurses. Often, the introduction of these concepts occurs primarily in postgraduate studies, leaving bachelor-level nurses less informed. Furthermore, the variety of theoretical frameworks and their differing levels of abstraction can make it challenging for nurses to select an appropriate functional theory [9, 11].
This scoping review aims to identify and categorize various rehabilitation nursing models. In health research, scoping reviews are becoming increasingly common as they effectively map studies conducted within a specific area and highlight evidence that aligns with the study’s objectives. In emerging fields such as rehabilitation sciences, where randomized controlled trials may be limited, scoping reviews are particularly valuable. They help researchers understand the existing landscape of literature and identify gaps in knowledge, thereby underscoring the importance of reviews in advancing the field [12, 13].
Despite their proven effectiveness, nursing theories remain underutilized in clinical practice. This limitation is mainly due to nurses’ unfamiliarity, particularly at the undergraduate level, and the challenges of selecting appropriate models because of their diversity and abstract nature. Considering this scientific gap and the lack of practical guidance in rehabilitation, scoping reviews can map the existing literature, identify knowledge gaps, and introduce applicable rehabilitation nursing models.
Objectives
The present study aimed to identify, categorize, and present specific rehabilitation nursing models through a scoping review of existing studies.
Methods
The scoping review methodology, as outlined by Arksey and O’Malley [12], is a widely accepted approach for mapping key concepts, types of evidence, and research gaps within a defined field. This method is particularly useful when the topic is broad or complex and has not been comprehensively reviewed before.
Study Design
The Arksey and O’Malley framework includes five main stages [12]:
1. Determining the research question
The research question guiding this study was: “What models have been designed or utilized in the field of rehabilitation nursing?”
2. Identifying relevant studies
To identify relevant studies, a review of the available literature was conducted using MeSH and Emtree terms to select the most effective keywords for the search.
3. Selection of related studies
Studies were selected based on their relevance to rehabilitation nursing theories and models.
4. Charting the data
A data extraction table was developed to show the purpose of the study, publication year, type of study, model, and main results.
5. Collecting and summarizing the findings
Findings were synthesized to identify key themes, patterns, and differences among the reviewed studies.
Search Strategy
The search was conducted using key English terms such as “model,” “theory,” “nursing care,” “nursing practice,” and “rehabilitation.” (Table 1).
Based on the inclusion criteria, the following databases were searched up to September 2024: Embase, PubMed, Cochrane, Web of Science, Scopus, ProQuest, and Google Scholar (Figure 1).
Following this, studies were manually reviewed, and a list of related articles and journals was compiled.
The nursing profession encompasses numerous theories developed by nursing theorists or adapted from related fields, which represent a significant aspect of the discipline [1, 2]. These theories are utilized by nurses across various domains, including clinical practice, research, education, and nursing management, thereby enhancing the overall quality of the nursing profession [1, 3, 4]. Evidence indicates that nurses who provide theory-based care achieve better clinical outcomes compared to those delivering traditional care, particularly in areas such as self-efficacy, patient self-care, and overall quality of life [3, 5]. Furthermore, these theories not only shape nurses’ performance but also contribute to their job satisfaction [3, 5, 6].
In complex specialties such as rehabilitation nursing, the diverse and specific needs of patients necessitate accurate identification of their requirements and the provision of comprehensive care [7, 8]. It is essential to recognize that nursing theories exist at various levels of abstraction; some highly abstract theories may restrict their practical application in nursing care. Conversely, theories that are more concrete and specific are better suited for direct nursing practice [1, 6]. Additionally, aligning nursing theories and models with fundamental nursing principles, such as those emphasized in rehabilitation nursing, enhances their clinical utility.
Despite the demonstrated positive effects of theory-based care on clinical outcomes [2, 9, 10], the application of these theories in clinical nursing remains limited, and many nurses exhibit reluctance to adopt them. This reluctance may stem from a lack of familiarity with nursing theories and models among clinical nurses. Often, the introduction of these concepts occurs primarily in postgraduate studies, leaving bachelor-level nurses less informed. Furthermore, the variety of theoretical frameworks and their differing levels of abstraction can make it challenging for nurses to select an appropriate functional theory [9, 11].
This scoping review aims to identify and categorize various rehabilitation nursing models. In health research, scoping reviews are becoming increasingly common as they effectively map studies conducted within a specific area and highlight evidence that aligns with the study’s objectives. In emerging fields such as rehabilitation sciences, where randomized controlled trials may be limited, scoping reviews are particularly valuable. They help researchers understand the existing landscape of literature and identify gaps in knowledge, thereby underscoring the importance of reviews in advancing the field [12, 13].
Despite their proven effectiveness, nursing theories remain underutilized in clinical practice. This limitation is mainly due to nurses’ unfamiliarity, particularly at the undergraduate level, and the challenges of selecting appropriate models because of their diversity and abstract nature. Considering this scientific gap and the lack of practical guidance in rehabilitation, scoping reviews can map the existing literature, identify knowledge gaps, and introduce applicable rehabilitation nursing models.
Objectives
The present study aimed to identify, categorize, and present specific rehabilitation nursing models through a scoping review of existing studies.
Methods
The scoping review methodology, as outlined by Arksey and O’Malley [12], is a widely accepted approach for mapping key concepts, types of evidence, and research gaps within a defined field. This method is particularly useful when the topic is broad or complex and has not been comprehensively reviewed before.
Study Design
The Arksey and O’Malley framework includes five main stages [12]:
1. Determining the research question
The research question guiding this study was: “What models have been designed or utilized in the field of rehabilitation nursing?”
2. Identifying relevant studies
To identify relevant studies, a review of the available literature was conducted using MeSH and Emtree terms to select the most effective keywords for the search.
3. Selection of related studies
Studies were selected based on their relevance to rehabilitation nursing theories and models.
4. Charting the data
A data extraction table was developed to show the purpose of the study, publication year, type of study, model, and main results.
5. Collecting and summarizing the findings
Findings were synthesized to identify key themes, patterns, and differences among the reviewed studies.
Search Strategy
The search was conducted using key English terms such as “model,” “theory,” “nursing care,” “nursing practice,” and “rehabilitation.” (Table 1).
Based on the inclusion criteria, the following databases were searched up to September 2024: Embase, PubMed, Cochrane, Web of Science, Scopus, ProQuest, and Google Scholar (Figure 1).
Following this, studies were manually reviewed, and a list of related articles and journals was compiled.
Table 1. Search Strategy and Results
| Database | Syntax |
| PubMed | (("nursing care"[Title/Abstract] OR "nursing practice"[Title/Abstract]) AND "rehabilitation"[Title/Abstract] AND ("model"[Title/Abstract] OR "theory"[Title/Abstract])) AND (english[Filter]) |
| Web of Science | ((((TI=(model)) OR TI=(theory)) OR AB=(model)) OR AB=(theory)) AND ((TI=(rehabilitation)) OR AB=(rehabilitation)) AND ((((TI=("nursing care")) OR TI=("nursing practice")) OR AB=("nursing practice")) OR AB=("nursing care")) and English (Languages) |
| Embase | ('model':ab,ti OR 'theory':ab,ti) AND 'rehabilitation':ab,ti AND ('nursing care':ab,ti OR 'nursing practice':ab,ti) |
| Scopus | ((TITLE-ABS-KEY ("nursing care") OR TITLE-ABS-KEY ("nursing practice")) AND TITLE-ABS-KEY (rehabilitation) AND (TITLE-ABS-KEY (model) OR TITLE-ABS-KEY (theory))) AND (LIMIT-TO (LANGUAGE, "English")) |
| ProQuest | (ab("nursing care") OR ti("nursing care") OR ab("nursing practice") OR ti("nursing practice")) AND (ab("rehabilitation") OR ti("rehabilitation")) AND (ab("model") OR ti("model") OR ab("theory") OR ti("theory")) English |
Inclusion and Exclusion Criteria
Articles published in English that directly addressed nursing care models in rehabilitation were included in the review. Studies were excluded if they lacked sufficient and reliable evidence regarding the models used, were written in languages other than English, had limited access to the full text, were presented only as oral presentations or speeches, or if the full-text PDF was unavailable (Table 2).
Articles published in English that directly addressed nursing care models in rehabilitation were included in the review. Studies were excluded if they lacked sufficient and reliable evidence regarding the models used, were written in languages other than English, had limited access to the full text, were presented only as oral presentations or speeches, or if the full-text PDF was unavailable (Table 2).
Table 2. Inclusion and Exclusion Criteria Based on the PICOS Framework
| Component | Description |
| Population (P) | Registered nurses, nursing students, or healthcare teams involved in providing rehabilitation care. |
| Intervention (I) | Application, description, evaluation, or development of nursing care models related to rehabilitation. |
| Comparison (C) | Studies with or without comparison to other care models or traditional approaches. |
| Outcomes (O) | Outcomes related to quality of care, patient recovery, functional improvement, professional performance, or interdisciplinary collaboration. |
| Study Design (S) | Qualitative, quantitative, mixed-method, or theoretical studies published in peer-reviewed journals. |
| Inclusion Criteria | - Studies published in English. - Full-text available. - Directly addressing nursing models in rehabilitation. |
| Exclusion Criteria | - Studies not explicitly related to rehabilitation nursing models. - Insufficient or unreliable evidence. - Non-English publications. - Lack of full-text access. - Abstracts, conference presentations, or speeches only. |
Study Selection
In the initial search, a total of 671 articles were identified. The selection process was conducted in two stages by two independent reviewers. In the first stage, titles and abstracts were screened to remove irrelevant studies, such as those that did not address nursing models or were unrelated to rehabilitation nursing. In the second stage, the full texts of 38 potentially relevant articles were reviewed in detail. Studies were excluded if they did not explicitly mention a nursing model, provided insufficient data about the model’s structure, or lacked clear methodological descriptions. Finally, 17 articles met the inclusion criteria and were included in the final analysis (Figure 1).
Data Extraction
A structured table was developed that included key information from each study, such as the purpose, year, type of study, theoretical or conceptual model used, and main findings. Additional columns were added for study setting, participants, country, and data collection methods. This comprehensive approach allowed for the identification of common themes, gaps, and trends.
Figure 1. PRISMA Flow Chart
Quality Appraisal
The methodological quality of the included studies was assessed using standardized appraisal tools appropriate for each study design. Randomized Controlled Trials (RCTs) were evaluated using the Cochrane Risk of Bias tool (RoB 2); qualitative studies were appraised using the CASP checklist; and case reports or series were assessed with the JBI Critical Appraisal Checklist.
Each study was independently reviewed by two researchers, and discrepancies were resolved through discussion and consensus.
While no studies were excluded solely based on quality, this appraisal informed the interpretation and synthesis of findings, highlighting methodological strengths and limitations.
Data Synthesis
A total of fourteen models related to rehabilitation nursing were identified and categorized into two main groups: general models and specific models.
General models were adapted from broader nursing or healthcare frameworks, while specific models were designed explicitly for rehabilitation nursing. This categorization clarified the theoretical diversity and evolution of conceptual approaches within the field.
Results
From the articles reviewed, a total of 17 studies were selected for the final analysis. Among these, five articles (29.4%) were published within the last five years [14–18], all in international journals, with seven articles (41.1%) specifically published in rehabilitation journals [7, 19–23].
In terms of levels of evidence, eight articles (47.5%) provided level IV evidence [7, 16, 17, 19, 22–25], while five articles (29.4%) provided level II evidence [14, 15, 20, 21, 26] (Table 3).
In thirteen articles (76.47%), the models were directly applied to patients with conditions requiring rehabilitation, such as heart attacks [17, 18, 27, 28], cerebrovascular accidents (CVAs) [14, 15, 20–23], spinal cord injuries [25], burns [26], and pulmonary disorders [16]. Additionally, three articles (17.64%) discussed the development of new models. A total of fourteen models were identified and categorized into general and specific models. Of these, nine originated from the field of general nursing, while five were specific to rehabilitation nursing.
Table 3. Specifications of Selected Studies
| Level of Scientific Evidence | Type of Study | Year of Publication | Location |
| IV | Case report | 1990 | England |
| — | Unclear | 1993 | USA |
| — | Unclear | 1994 | USA |
| I | Review | 2004 | Finland |
| IV | Qualitative-grand theory | 2006 | USA |
| IV | Qualitative-content analysis | 2007 | Canada |
| IV | Qualitative-grand theory | 2007 | Taiwan |
| II | Quantitative-semi-experimental | 2014 | Iran |
| II | Quantitative-randomized controlled intervention | 2017 | China |
| II | Quantitative-randomized controlled clinical trial | 2020 | China |
| II | Quantitative-futuristic randomized controlled study | 2021 | China |
| IV | Case report | 2021 | Turkey |
| IV | Theoretical development study | 2021 | Brazil |
| IV | Case report | 1993 | USA |
| IV | Qualitative-content analysis | 1994 | USA |
| III | Retrospective study | 2019 | Italy |
| II | Quantitative-semi-experimental | 2014 | Iran |
From the nursing field, four models were foundational nursing theories:
- Gordon’s Functional Health Pattern Model [27]
- Bandura’s Self-Efficacy Theory [27]
- Psychosocial Biology [26]
- Interactive Standard Theory [15]
- Collaborative Care Model [14]
- Social Support Theory [23]
- Geriatric Rehabilitation Nursing Model
- Mauk Model for Poststroke Recovery
- Provision of Nursing Care for the Rehabilitation of the Elderly
- Super-Link System Theory
- Middle-Range Theory for Cardiovascular Rehabilitation Nursing (Table 4).
Among the reviewed articles, two (11.7%) did not specify their methodology, and one (5%) did not indicate the source of the model used, although it referred to common frameworks in rehabilitation nursing. This lack of specification was noted for completeness.
Discussion
This scoping review of 17 articles revealed that rehabilitation nursing models enable nurses to provide patient-centered, high-quality care for individuals with disabilities and their families, thereby improving health outcomes and quality of life. Various models in rehabilitation nursing are designed to address the complex needs of patients with chronic or special conditions, such as cerebrovascular accidents, cardiovascular diseases, burns, spinal cord injuries, and pulmonary disorders. These models offer structured approaches to guide nursing practice, enhance patient engagement, and support holistic care planning.
The review identified fourteen models in total, categorized into general and specific models. General models, such as Roy’s Adaptation Model, Orem’s Self-Care Model, Pender’s Health Promotion Model, and Gordon’s Functional Health Model, were adapted from broader nursing or interdisciplinary frameworks. These models emphasize essential aspects of patient care, including adaptation, self-care, motivation, behavioral change, and health promotion, making them versatile tools across various clinical settings.
Specific models, including the Mauk Model for Poststroke Recovery, Geriatric Rehabilitation Nursing Model, Nursing Care Delivery Model for Geriatric Rehabilitation, Super-Link System Theory, and Middle-Range Theory for Cardiovascular Rehabilitation Nursing, were developed explicitly for rehabilitation contexts, offering targeted guidance for specialized patient populations [30, 31].
Analysis of the included studies indicated that most models (76.47%) were directly applied to patients, demonstrating their practical utility in clinical settings. These applications highlight the ability of models to inform individualized interventions, structure care delivery, improve communication within multidisciplinary teams, and promote family involvement.
Among the general models, Roy’s Adaptation Model and Orem’s Self-Care Model demonstrated the highest adaptability across different patient populations and clinical contexts. Their flexibility stems from their focus on universal concepts such as adaptation, coping mechanisms, and self-management, which can be tailored to diverse conditions ranging from cardiovascular rehabilitation to stroke recovery and geriatric care. Similarly, Pender’s Health Promotion Model proved adaptable due to its emphasis on behavioral motivation and patient empowerment, applicable across multiple rehabilitation scenarios [3, 16].
In contrast, specific models, although highly effective within their targeted populations, may require modifications for application to different clinical conditions. For instance, models such as Mauk’s Poststroke Recovery Model or the Super-Link System Theory provide structured frameworks for specific rehabilitation contexts but are not universally transferable without adaptation [15, 25].
Table 4. Specifications of Selected Studies
Discussion
This scoping review of 17 articles revealed that rehabilitation nursing models enable nurses to provide patient-centered, high-quality care for individuals with disabilities and their families, thereby improving health outcomes and quality of life. Various models in rehabilitation nursing are designed to address the complex needs of patients with chronic or special conditions, such as cerebrovascular accidents, cardiovascular diseases, burns, spinal cord injuries, and pulmonary disorders. These models offer structured approaches to guide nursing practice, enhance patient engagement, and support holistic care planning.
The review identified fourteen models in total, categorized into general and specific models. General models, such as Roy’s Adaptation Model, Orem’s Self-Care Model, Pender’s Health Promotion Model, and Gordon’s Functional Health Model, were adapted from broader nursing or interdisciplinary frameworks. These models emphasize essential aspects of patient care, including adaptation, self-care, motivation, behavioral change, and health promotion, making them versatile tools across various clinical settings.
Specific models, including the Mauk Model for Poststroke Recovery, Geriatric Rehabilitation Nursing Model, Nursing Care Delivery Model for Geriatric Rehabilitation, Super-Link System Theory, and Middle-Range Theory for Cardiovascular Rehabilitation Nursing, were developed explicitly for rehabilitation contexts, offering targeted guidance for specialized patient populations [30, 31].
Analysis of the included studies indicated that most models (76.47%) were directly applied to patients, demonstrating their practical utility in clinical settings. These applications highlight the ability of models to inform individualized interventions, structure care delivery, improve communication within multidisciplinary teams, and promote family involvement.
Among the general models, Roy’s Adaptation Model and Orem’s Self-Care Model demonstrated the highest adaptability across different patient populations and clinical contexts. Their flexibility stems from their focus on universal concepts such as adaptation, coping mechanisms, and self-management, which can be tailored to diverse conditions ranging from cardiovascular rehabilitation to stroke recovery and geriatric care. Similarly, Pender’s Health Promotion Model proved adaptable due to its emphasis on behavioral motivation and patient empowerment, applicable across multiple rehabilitation scenarios [3, 16].
In contrast, specific models, although highly effective within their targeted populations, may require modifications for application to different clinical conditions. For instance, models such as Mauk’s Poststroke Recovery Model or the Super-Link System Theory provide structured frameworks for specific rehabilitation contexts but are not universally transferable without adaptation [15, 25].
Table 4. Specifications of Selected Studies
| Results | Model | Purpose of the Study | Title | First Author |
| Roy’s Adaptation Model serves as a valuable framework for rehabilitation nursing practice. Patients undergoing rehabilitation often experience changes in physiological roles, interdependence, and self-concept. This model provides a holistic approach that promotes patient integrity and potential. | Roy's Adaptation Model | Designing the nursing process based on Roy's model | Roy's adaptation model: a guide for rehabilitation nursing practice | Piazza [19] |
| Self-efficacy assessment helps nurses identify if patients are struggling to manage cardiovascular risk factors. Specific training and counseling during and after discharge are recommended. | Bandura's Self-Efficacy Theory | Provide evaluation and intervention strategies used by clinical nurses | Advanced rehabilitation nursing care of coronary angioplasty patients using self-efficacy theory | Jensen [28] |
| Bandura’s self-efficacy theory offers a systematic framework for interpreting, modifying, and predicting patient behaviors. | Bandura's Self-Efficacy Theory | Describe development and conceptual framework; apply to cardiac rehabilitation | Bandura's self-efficacy theory: a guide for cardiac rehabilitation nursing practice | Jeng [27] |
| The Geriatric Rehabilitation Nursing Model provides useful tools for improving nursing care, documentation, and communication with healthcare teams. | Geriatric Rehabilitation Nursing Model | Describe a geriatric rehabilitation nursing model developed from nursing and rehabilitation texts | Geriatric rehabilitation nursing: developing a model | Routasalo [29] |
| The Mauk Model helps nurses identify the stage of post-stroke recovery and tailor care accordingly. | Mauk Model for Poststroke Recovery | Apply the Mauk model to stroke rehabilitation across six recovery stages | Nursing interventions within the Mauk model of poststroke recovery | Mauk [22] |
| The Nursing Care Delivery Model defines the role and responsibility of geriatric rehabilitation nurses. | Nursing Care Delivery Model for Geriatric Rehabilitation | Design a care delivery model for geriatric rehabilitation | Practice change: developing and implementing a nursing care delivery model for geriatric rehabilitation | Cormack [24] |
| The Super-Link System Theory helps nurses organize rehabilitation care for spinal cord injury patients, linking theory to practice. | Super-Link System Theory | Identify patient and family needs during rehabilitation | Establishing a super-link system: spinal cord injury rehabilitation nursing | Chen [25] |
| The Mauk Model increased stroke patients’ adaptation following training interventions. | Mauk Model for Poststroke Recovery | Determine the impact of implementing the Mauk rehabilitation nursing model on stroke patient compliance | Implication of the Mauk nursing rehabilitation model on adjustment of stroke patients | Ibrahimpour [21] |
| Rehabilitation interventions based on the psychosocial-biological model improved the overall health status of burn patients. | Biopsychosocial Rehabilitation Model | Evaluate the effect of rehabilitation interventions on the health of burn patients | Effect of a rehabilitation nursing intervention model on hand burn patients |
| Li [26] |
Evidence levels varied across the reviewed studies, with nearly half providing level IV evidence and fewer offering higher-level (level II) studies. This underscores the need for more rigorous research to validate the effectiveness of rehabilitation nursing models and their impact on measurable patient outcomes. Moreover, the findings reveal persistent gaps such as fragmented information, limited theoretical integration, and a notable theory–practice gap in rehabilitation nursing [5, 8, 14].
Many existing models remain highly specialized, which limits their broader applicability and scalability. Furthermore, the lack of standardized evaluation tools and insufficient training on theory-based practice among nurses contribute to the underutilization of these models in real-world clinical environments [9, 10].
Overall, the findings indicate that rehabilitation nursing relies on a combination of general and specific models to guide practice. Strengthening the evidence base, enhancing methodological rigor, and developing flexible, context-specific models are essential steps to improve theoretical integration, guide clinical decision-making, and advance patient-centered rehabilitation care. Future research should aim to evaluate these models in diverse cultural and clinical contexts, explore their effectiveness in multidisciplinary settings, and identify strategies to bridge the gap between theory and practice
Conclusion
This review highlights that rehabilitation nursing models are essential for improving care quality and patient outcomes by addressing patients’ physical, psychological, and social needs. General models, such as Roy’s Adaptation Model and Orem’s Self-Care Model, demonstrate high adaptability across diverse patient populations, while specific models, including the Mauk Model for Poststroke Recovery and the Geriatric Rehabilitation Nursing Model, provide targeted frameworks for specialized rehabilitation care.
Despite their demonstrated benefits, many models remain underutilized in practice, with limited high-level evidence and inconsistent integration into clinical routines. To advance rehabilitation nursing, future research should focus on developing context-specific models for various patient groups, exploring strategies to bridge the theory–practice gap, integrating digital tools and tele-rehabilitation for enhanced self-management, and evaluating barriers and facilitators to implementation in real-world clinical settings.
Addressing these priorities can enhance evidence-based, patient-centered care, strengthen interdisciplinary collaboration, and improve functional and quality-of-life outcomes for patients with complex rehabilitation needs.
Ethical Considerations
This study was a scoping review of previously published articles and did not involve direct participation of human subjects. Therefore, ethical approval and informed consent were not required. All included studies were properly cited to acknowledge the original authors and their work.
Acknowledgments
The authors would like to thank the Department of Nursing at the University of Social Welfare and Rehabilitation Sciences for their continuous guidance and academic support.
Conflict of Interest
The authors declare that there are no conflicts of interest related to this study.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors’ Contributions
Shirozhan Sh. and Shoja M. contributed to the conceptualization and design of the study.
Metanat F. and Motie M. were responsible for data collection, analysis, and interpretation.
Motie M. led the drafting and critical revision of the manuscript.
All authors reviewed and approved the final version of the manuscript and agreed to be accountable for all aspects of the work.
Artificial Intelligence Utilization for Article Writing
No artificial intelligence tools were used in the writing, analysis, or preparation of this manuscript. All content and decisions were solely performed by the authors.
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary materials.
The data supporting the findings of this study are available from the corresponding author upon reasonable
Type of Study: Review Articels |
Subject:
Nursing
References
1. Meleis AI. Theoretical Nursing: Development and Progress. Wolters Kluwer Health/Lippincott Williams & Wilkins; 2011. p. 470-480.
2. Arif S, Ali A, Hussain N. Nursing Theories: Foundation of Nursing Profession. i-Manager's Journal on Nursing. 2019;9(4):45. [https://doi.org/10.26634/jnur.9.4.16643]
3. Younas A, Quennell S. Usefulness of nursing theory-guided practice: an integrative review. Scandinavian Journal of Caring Sciences. 2019;33(3):540-55. [https://doi.org/10.1111/scs.12670] [PMID]
4. Arif S, Nasir A. Experiences of BSN students regarding application of nursing theories at clinical. Journal of Liaquat University of Medical & Health Sciences. 2019;18(3):241-4. [https://doi.org/10.22442/jlumhs.191830635]
5. Veo P. Concept mapping for applying theory to nursing practice. Journal for Nurses in Professional Development. 2010;26(1):17-22. [https://doi.org/10.1097/NND.0b013e3181cc2d6f] [PMID]
6. Kitson AL. The fundamentals of care framework as a point-of-care nursing theory. Nursing Research. 2018;67(2):99-107. [https://doi.org/10.1097/NNR.0000000000000271] [PMID]
7. Closson BL, Mattingly LJ, Finne KM, Larson JA. Telephone follow-up program evaluation: application of Orem's self-care model. Rehabilitation Nursing Journal. 1994;19(5):287-92. [https://doi.org/10.1002/j.2048-7940.1994.tb00824.x] [PMID]
8. Wang R, Duan G, Xu H, Wu Y, Su Y, Li J, et al. Analysis on the effect of the rehabilitation intervention-centered targeted nursing model on cardiac function recovery and negative emotions in patients with acute myocardial infarction. Journal of Healthcare Engineering. 2022;2022(1):1246092. [https://doi.org/10.1155/2022/1246092] [PMID]
9. Mohammadi E, Abbasi K, Saadati M. Barriers to implementation of nursing theories in clinical practice from the perspective of nurses. Iranian Journal of Nursing Research. 2015;10(1):13-24. [http://ijnr.ir/article-1-1477-en.html]
10. Pashaeypoor S, Baumann SL, Sadat Hoseini A, Cheraghi MA, Chenari HA. Identifying and overcoming barriers for implementing Watson's human caring science. Nursing Science Quarterly. 2019;32(3):239-44. [https://doi.org/10.1177/0894318419845396] [PMID]
11. Shirozhan S, Arsalani N, Seyed Bagher Maddah S, Mohammadi-Shahboulaghi F. Barriers and facilitators of rehabilitation nursing care for patients with disability: a qualitative study. Frontiers in Public Health. 2022;10:931287. [https://doi.org/10.3389/fpubh.2022.931287] [PMID]
12. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19-32. [https://doi.org/10.1080/1364557032000119616]
13. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implementation Science. 2010;5:1-9. [https://doi.org/10.1186/1748-5908-5-69] [PMID]
14. Wu Z, Xu J, Yue C, Li Y, Liang Y. Collaborative Care Model-Based Telerehabilitation Exercise Training Program for Acute Stroke Patients in China: A Randomized Controlled Trial. Journal of Stroke and Cerebrovascular Diseases. 2020;29(12):105328. [https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105328] [PMID]
15. Li N, Wang J, Zheng M, Ge Q. Application Value of Rehabilitation Nursing in Patients with Stroke Based on the Theory of Interactive Standard: A Randomized Controlled Study. Evidence-Based Complementary and Alternative Medicine. 2021;2021:9452765. [https://doi.org/10.1155/2021/9452765] [PMID]
16. Otu M, Karagozoglu S. Nursing Care Based on Health Promotion Model in Patients with Overlap Syndrome within the Scope of Pulmonary Rehabilitation: Case Report. International Journal of Caring Sciences. 2021;14(3):2046-2054. [https://internationaljournalofcaringsciences.org/docs/55_otu_special_14_3.pdf]
17. Farias MS, Silva LdFd, Brandão MAG, Guedes MVC, Pontes KMdA, Lopes ROP. Medium Reach Theory for Nursing in Cardiovascular Rehabilitation. Revista Brasileira de Enfermagem. 2021;74(3):e20190718. [https://doi.org/10.1590/0034-7167-2019-0718] [PMID]
18. Iannicelli AM, De Matteo P, Vito D, Pellecchia E, Dodaro C, Giallauria F, et al. Use of the North American Nursing Diagnosis Association Taxonomies, Nursing Intervention Classification, Nursing Outcomes Classification, and NANDA-NIC-NOC Linkage in Cardiac Rehabilitation. Monaldi Archives for Chest Disease. 2019;89(2). [https://doi.org/10.4081/monaldi.2019.1060] [PMID]
19. Piazza D, Foote A. Roy's Adaptation Model: A Guide for Rehabilitation Nursing Practice. Rehabilitation Nursing. 1990;15(5):254-259. [https://doi.org/10.1002/j.2048-7940.1990.tb01488.x] [PMID]
20. Shoja M, Dalvandi A, Tafakhori A, Sarraf P, Kazemi R, Ebrahimpour Z, et al. Implication of the Mauk Nursing Intervention Model on Coping Strategies of Stroke Survivors. Iranian Rehabilitation Journal. 2015;13(2):51-56. [http://irj.uswr.ac.ir/article-1-392-en.html]
21. Dalvandi A, Khankeh H, Kazemi R, Tafakhori A, Sarraf P, Biglarian A, et al. Implication of the Mauk Nursing Rehabilitation Model on the Adjustment of Stroke Patients. Iranian Rehabilitation Journal. 2014;12(4):6-10. [http://irj.uswr.ac.ir/article-1-391-en.html]
22. Mauk KL. Nursing Interventions within the Mauk Model of Poststroke Recovery. Rehabilitation Nursing Journal. 2006;31(6):257-264. [https://doi.org/10.1002/j.2048-7940.2006.tb00022.x] [PMID]
23. Ragsdale D, Yarbrough S, Lasher AT. Using Social Support Theory to Care for CVA Patients. Rehabilitation Nursing. 1993;18(3):154-161. [https://doi.org/10.1002/j.2048-7940.1993.tb00744.x] [PMID]
24. Cormack C, Hillier LM, Anderson K, Cheeseman A, Clift J, Fisher M-J, et al. Practice Change: The Process of Developing and Implementing a Nursing Care Delivery Model for Geriatric Rehabilitation. Journal of Nursing Administration. 2007;37(6):279-286. [https://doi.org/10.1097/01.NNA.0000277719.79876.ec] [PMID]
25. Chen HY, Boore JR. Establishing a Super-Link System: Spinal Cord Injury Rehabilitation Nursing. Journal of Advanced Nursing. 2007;57(6):639-648. [https://doi.org/10.1111/j.1365-2648.2006.04160.x] [PMID]
26. Li L, Dai J-x, Xu L, Huang Z-x, Pan Q, Zhang X, et al. The Effect of a Rehabilitation Nursing Intervention Model on Improving the Comprehensive Health Status of Patients with Hand Burns. Burns. 2017;43(4):877-885. [https://doi.org/10.1016/j.burns.2016.11.003] [PMID]
27. Jeng C, Braun LT. Bandura's Self-Efficacy Theory: A Guide for Cardiac Rehabilitation Nursing Practice. Journal of Holistic Nursing. 1994;12(4):425-436. [https://doi.org/10.1177/089801019401200411] [PMID]
28. Jensen K, Banwart L, Venhaus R, Popkess-Vawter S, Perkins SB. Advanced Rehabilitation Nursing Care of Coronary Angioplasty Patients Using Self-Efficacy Theory. Journal of Advanced Nursing. 1993;18(6):926-931. [https://doi.org/10.1046/j.1365-2648.1993.18060926.x] [PMID]
29. Routasalo P, Arve S, Lauri S. Geriatric Rehabilitation Nursing: Developing a Model. International Journal of Nursing Practice. 2004;10(5):207-215. [https://doi.org/10.1111/j.1440-172X.2004.00480.x] [PMID]
30. Roy C, Roberts SL. Theory Construction in Nursing: An Adaptation Model. 1981. p. 31-48. [https://books.google.com/books/about/Theory_Construction_in_Nursing.html?id=vwJtAAAAMAAJ]
31. Pender NJ. Health Promotion Model Manual. 2011. [https://www.scirp.org/reference/referencespapers?referenceid=2406627]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




