Preventive Care in Nursing and Midwifery Journal

Volume 15, Issue 3 (10-2025)
Prev Care Nurs Midwifery J 2025, 15(3): 80-90 |
Back to browse issues page
Ethics code: IR.LARUMS.REC.1402.016
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bazrafshan M, Barghi O, Mansouri A, modarresi M, Masmouei B. Policy insights into nutritional decision-making in individuals with metabolic syndrome: Implications for food labeling and dietary choices. Prev Care Nurs Midwifery J 2025; 15 (3) :80-90
URL: http://nmcjournal.zums.ac.ir/article-1-993-en.html
URL: http://nmcjournal.zums.ac.ir/article-1-993-en.html
Mohammad-Rafi Bazrafshan 

 , Omid Barghi
, Omid Barghi 

 , Amir Mansouri
, Amir Mansouri 

 , MohammadJavad Modarresi
, MohammadJavad Modarresi 

 , Behnam Masmouei *
, Behnam Masmouei * 




 , Omid Barghi
, Omid Barghi 

 , Amir Mansouri
, Amir Mansouri 

 , MohammadJavad Modarresi
, MohammadJavad Modarresi 

 , Behnam Masmouei *
, Behnam Masmouei * 


School of Nursing Hazrat Zahra (P.B.U.H) Abadeh, Shiraz University of Medical Sciences, Shiraz, Iran. , behnam.masmouei@gmail.com
Abstract: (145 Views)
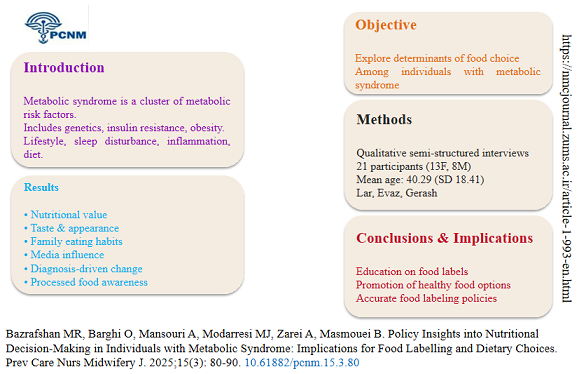
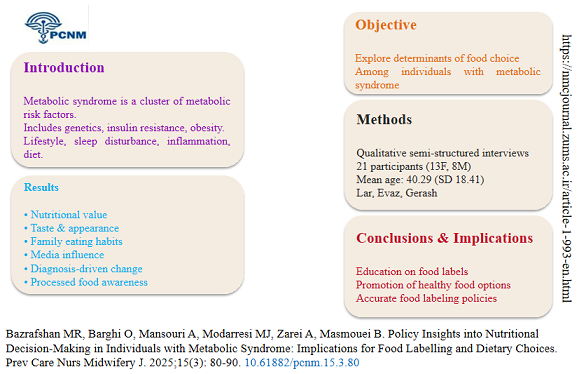
Background: Metabolic syndrome is a cluster of metabolic risk factors associated with a multitude of determinants, including genetics, insulin resistance, adverse lifestyle habits, sleep disturbances, chronic inflammation, fetal and neonatal complications, circadian rhythm disruptions, obesity, and dietary patterns.
Objectives: This qualitative study aimed to explore the determinants of food choices among individuals diagnosed with metabolic syndrome.
Methods: Data were collected using a qualitative design and semi-structured interviews. Participants were recruited through purposive sampling from community health centers in the cities of Lar, Evaz, and Gerash. The sample consisted of 21 individuals (13 females and 8 males) with a confirmed diagnosis of metabolic syndrome, with a mean age of 40.29 years (SD = 18.41).
Results: The analysis identified several key themes influencing food selection: considerations of nutritional value, the influence of taste and food appearance, conflicts regarding family dietary habits, the impact of media, dietary modifications driven by disease diagnosis, and awareness of processed foods. Participants highlighted the significance of nutritional information and expressed concerns about the accuracy of food labels.
Conclusions: The findings underscore the complex interplay of factors shaping the dietary decisions of individuals with metabolic syndrome. Key implications for practice include educating this population on how to interpret food labels accurately and promoting healthier food options. Furthermore, ensuring the veracity of food labeling is critical, as it can empower individuals to make informed dietary choices, thereby potentially mitigating the prevalence and burden of metabolic syndrome.
Objectives: This qualitative study aimed to explore the determinants of food choices among individuals diagnosed with metabolic syndrome.
Methods: Data were collected using a qualitative design and semi-structured interviews. Participants were recruited through purposive sampling from community health centers in the cities of Lar, Evaz, and Gerash. The sample consisted of 21 individuals (13 females and 8 males) with a confirmed diagnosis of metabolic syndrome, with a mean age of 40.29 years (SD = 18.41).
Results: The analysis identified several key themes influencing food selection: considerations of nutritional value, the influence of taste and food appearance, conflicts regarding family dietary habits, the impact of media, dietary modifications driven by disease diagnosis, and awareness of processed foods. Participants highlighted the significance of nutritional information and expressed concerns about the accuracy of food labels.
Conclusions: The findings underscore the complex interplay of factors shaping the dietary decisions of individuals with metabolic syndrome. Key implications for practice include educating this population on how to interpret food labels accurately and promoting healthier food options. Furthermore, ensuring the veracity of food labeling is critical, as it can empower individuals to make informed dietary choices, thereby potentially mitigating the prevalence and burden of metabolic syndrome.
Keywords: Metabolic Syndrome, Food Labeling, Nutritional Decision-Making, Qualitative Study, Policy Brief
Full-Text [PDF 802 kb]
(94 Downloads)
| | Full-Text (HTML) (3 Views)
Knowledge Translation Statement
Audience: Public health nurses, clinical dietitians, primary care providers, and health policymakers
Policy-level tools, such as clear and comprehensible food labeling, are crucial for supporting individuals with metabolic Syndrome in making informed dietary choices. Integrating evidence-based nutritional guidance into straightforward labeling and public health messaging can empower patients and bridge the gap between clinical dietary advice and everyday food selection, thereby improving disease management and health outcomes.
Audience: Public health nurses, clinical dietitians, primary care providers, and health policymakers
Policy-level tools, such as clear and comprehensible food labeling, are crucial for supporting individuals with metabolic Syndrome in making informed dietary choices. Integrating evidence-based nutritional guidance into straightforward labeling and public health messaging can empower patients and bridge the gap between clinical dietary advice and everyday food selection, thereby improving disease management and health outcomes.
Type of Study: Orginal research |
Subject:
Nursing
References
1. Castro-Barquero S, Ruiz-León AM, Sierra-Pérez M, Estruch R, Casas R. Dietary Strategies for Metabolic Syndrome: A Comprehensive Review. Nutrients. 2020 Oct;12(10):2983. [https://doi.org/10.3390/nu12102983] [PMID]
2. Law J, Martin E. Concise Medical Dictionary. 10th ed. Oxford: Oxford University Press; 2020. [https://doi.org/10.1093/acref/9780198836612.001.0001]
3. Nilsson PM, Tuomilehto J, Rydén L. The Metabolic Syndrome - What Is It and How Should It Be Managed? European Journal of Preventive Cardiology. 2019 Jun;26(2_suppl):33-46. [https://doi.org/10.1177/2047487319886404] [PMID]
4. Paley CA, Johnson MI. Abdominal Obesity and Metabolic Syndrome: Exercise as Medicine? BMC Sports Science, Medicine and Rehabilitation. 2018 Dec;10(1):7. [https://doi.org/10.1186/s13102-018-0097-1] [PMID]
5. Kahn CR, Wang G, Lee KY. Altered Adipose Tissue and Adipocyte Function in the Pathogenesis of Metabolic Syndrome. The Journal of Clinical Investigation. 2019 Oct;129(10):3990-4000. [https://doi.org/10.1172/JCI129187] [PMID]
6. Ferns GA, Ghayour-Mobarhan M. Metabolic Syndrome in Iran: A Review. Translational Metabolic Syndrome Research. 2018 Dec;1:10-22. [https://doi.org/10.1016/j.tmsr.2018.04.001]
7. Finicelli M, Squillaro T, Di Cristo F, Di Salle A, Melone MAB, Galderisi U, et al. Metabolic Syndrome, Mediterranean Diet, and Polyphenols: Evidence and Perspectives. Journal of Cellular Physiology. 2019 May;234(5):5807-26. [https://doi.org/10.1002/jcp.27506] [PMID]
8. Salas-Salvadó J, Guasch-Ferré M, Lee CH, Estruch R, Clish CB, Ros E. Protective Effects of the Mediterranean Diet on Type 2 Diabetes and Metabolic Syndrome. The Journal of Nutrition. 2016 Apr;146(4):920S-927S. [https://doi.org/10.3945/jn.115.218487] [PMID]
9. Lackey DE, Lazaro RG, Li P, Johnson A, Hernandez-Carretero A, Weber N, et al. The Role of Dietary Fat in Obesity-Induced Insulin Resistance. American Journal of Physiology-Endocrinology and Metabolism. 2016 Dec;311(6):E989-E997. [https://doi.org/10.1152/ajpendo.00323.2016] [PMID]
10. Wang T, Heianza Y, Sun D, Huang T, Ma W, Rimm EB, et al. Improving Adherence to Healthy Dietary Patterns, Genetic Risk, and Long Term Weight Gain: Gene-Diet Interaction Analysis in Two Prospective Cohort Studies. BMJ. 2018 Mar;360:j5644. [https://doi.org/10.1136/bmj.j5644] [PMID]
11. Grosso G, Galvano F. Mediterranean Diet Adherence in Children and Adolescents in Southern European Countries. NFS Journal. 2016 Mar;3:13-9. [https://doi.org/10.1016/j.nfs.2016.02.004]
12. Shangguan S, Afshin A, Shulkin M, Ma W, Marsden D, Smith J, et al. A Meta-Analysis of Food Labeling Effects on Consumer Diet Behaviors and Industry Practices. American Journal of Preventive Medicine. 2019 Feb;56(2):300-14. [https://doi.org/10.1016/j.amepre.2018.09.024] [PMID]
13. Gregori D, Ballali S, Vögele C, Galasso F, Widhalm K, Berchialla P, et al. What Is the Value Given by Consumers to Nutritional Label Information? Results from a Large Investigation in Europe. Journal of the American College of Nutrition. 2015;34(2):120-5. [https://doi.org/10.1080/07315724.2014.899936] [PMID]
14. Sánchez-García I, Rodríguez-Insuasti H, Martí-Parreño J, Sánchez-Mena A. Nutritional Traffic Light and Self-Regulatory Consumption: The Role of Emotions. British Food Journal. 2019 Jan;121(1):183-98. [https://doi.org/10.1108/BFJ-03-2018-0192]
15. Vears DF, Gillam L. Inductive Content Analysis: A Guide for Beginning Qualitative Researchers. Focus on Health Professional Education: A Multi-Professional Journal. 2022 Mar;23(1):111-27. [https://doi.org/10.11157/fohpe.v23i1.544]
16. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Circulation. 2002 Dec;106(25):3143-421. [https://doi.org/10.1161/circ.106.25.3143] [PMID]
17. Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in Qualitative Research: Exploring Its Conceptualization and Operationalization. Quality & Quantity. 2018 Jul;52(4):1893-907. [https://doi.org/10.1007/s11135-017-0574-8] [PMID]
18. Graneheim UH, Lundman B. Qualitative Content Analysis in Nursing Research: Concepts, Procedures and Measures to Achieve Trustworthiness. Nurse Education Today. 2004 Feb;24(2):105-12. [https://doi.org/10.1016/j.nedt.2003.10.001] [PMID]
19. Enworo OC. Application of Guba and Lincoln's Parallel Criteria to Assess Trustworthiness of Qualitative Research on Indigenous Social Protection Systems. Qualitative Research Journal. 2023 Nov;23(4):372-84. [https://doi.org/10.1108/QRJ-08-2022-0116]
20. Chen PJ, Antonelli M. Conceptual Models of Food Choice: Influential Factors Related to Foods, Individual Differences, and Society. Foods. 2020 Dec;9(12):1898. [https://doi.org/10.3390/foods9121898] [PMID]
21. Leng G, Adan RA, Belot M, Brunstrom JM, De Graaf K, Dickson SL, et al. The Determinants of Food Choice. Proceedings of the Nutrition Society. 2017 Aug;76(3):316-27. [https://doi.org/10.1017/S002966511600286X] [PMID]
22. Zikankuba VL, Mwanyika G, Ntwenya JE, James A. Pesticide Regulations and Their Malpractice Implications on Food and Environment Safety. Cogent Food & Agriculture. 2019 Jan;5(1):1601544. [https://doi.org/10.1080/23311932.2019.1601544]
23. Saklayen MG. The Global Epidemic of the Metabolic Syndrome. Current Hypertension Reports. 2018 Feb;20(2):12. [https://doi.org/10.1007/s11906-018-0812-z] [PMID]
24. Ma G. Food, Eating Behavior, and Culture in Chinese Society. Journal of Ethnic Foods. 2015 Dec;2(4):195-9. [https://doi.org/10.1016/j.jef.2015.11.004]
25. Handford CE, Campbell K, Elliott CT. Impacts of Milk Fraud on Food Safety and Nutrition with Special Emphasis on Developing Countries. Comprehensive Reviews in Food Science and Food Safety. 2016 Jan;15(1):130-42. [https://doi.org/10.1111/1541-4337.12181] [PMID]
26. Nelson AM, Fleming R. Gender Differences in Diet and Social Media: An Explorative Study. Appetite. 2019 Oct;142:104383. [https://doi.org/10.1016/j.appet.2019.104383] [PMID]
27. Lin Y, Ying YY, Li SX, Wang SJ, Gong QH, Li H. Association between Alcohol Consumption and Metabolic Syndrome among Chinese Adults. Public Health Nutrition. 2021 Oct;24(14):4582-90. [https://doi.org/10.1017/S1368980020004449] [PMID]
28. Styne DM, Arslanian SA, Connor EL, Farooqi IS, Murad MH, Silverstein JH, et al. Pediatric Obesity-Assessment, Treatment, and Prevention: An Endocrine Society Clinical Practice Guideline. The Journal of Clinical Endocrinology & Metabolism. 2017 Mar;102(3):709-57. [https://doi.org/10.1210/jc.2016-2573] [PMID]
29. Kim OY, Kwak SY, Kim B, Kim YS, Kim HY, Shin MJ. Selected Food Consumption Mediates the Association between Education Level and Metabolic Syndrome in Korean Adults. Annals of Nutrition and Metabolism. 2017 May;70(2):122-31. [https://doi.org/10.1159/000470853] [PMID]
30. Egnell M, Crosetto P, d'Almeida T, Kesse-Guyot E, Touvier M, Ruffieux B, et al. Modelling the Impact of Different Front-of-Package Nutrition Labels on Mortality from Non-Communicable Chronic Disease. International Journal of Behavioral Nutrition and Physical Activity. 2019 May;16(1):56. [https://doi.org/10.1186/s12966-019-0817-2] [PMID]
31. de Morais Sato P, Mais LA, Khandpur N, Ulian MD, Bortoletto Martins AP, Garcia MT, et al. Consumers' Opinions on Warning Labels on Food Packages: A Qualitative Study in Brazil. PLoS One. 2019 Jun;14(6):e0218813. [https://doi.org/10.1371/journal.pone.0218813] [PMID]
32. John OD, du Preez R, Panchal SK, Brown L. Tropical Foods as Functional Foods for Metabolic Syndrome. Food & Function. 2020 Aug;11(8):6946-60. [https://doi.org/10.1039/D0FO01133A] [PMID]
33. Baudry J, Lelong H, Adriouch S, Julia C, Allès B, Hercberg S, et al. Association between Organic Food Consumption and Metabolic Syndrome: Cross-Sectional Results from the NutriNet-Santé Study. European Journal of Nutrition. 2018 Dec;57(7):2477-88. [https://doi.org/10.1007/s00394-017-1520-1] [PMID]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |