
Preventive Care in Nursing and Midwifery Journal

Volume 15, Issue 1 (1-2025)
Prev Care Nurs Midwifery J 2025, 15(1): 22-29 |
Back to browse issues page
Ethics code: IR.ZUMS.REC.1398.041
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pourrahimi A, Keshavarz Afshar M, Dezhgam N, Rohani B, Taghiloo H. Comparison of the quality of life of elderly men and women residing in nursing homes in the city of zanjan. Prev Care Nurs Midwifery J 2025; 15 (1) :22-29
URL: http://nmcjournal.zums.ac.ir/article-1-943-en.html
URL: http://nmcjournal.zums.ac.ir/article-1-943-en.html
Department of Operating Room and Anesthesiology, School of Nursing and Midwifery, Zanjan University of Medical Sciences, Zanjan, Iran , Taghiloo1372@zums.ac.ir
Abstract: (1198 Views)
Background: Quality of life serves as a helpful indicator for identifying the health and well-being of elderly people and also a criterion for evaluating the efficacy of the quality of care provided.
Objectives: The present research aimed to determine and compare the quality of life in elderly men and women residing in nursing homes.
Methods: This cross-sectional study was conducted on 110 elderly men and women residing in nursing homes in Zanjan province. Sampling was carried out through a convenience sampling method. The tools used in this study comprised a demographic information questionnaire and the Leiden-Padua (LEIPAD) Quality of Life Questionnaire. Data were analyzed using SPSS 20 software. The mean (standard deviation [SD]) and frequency (percentage) were used for descriptive statistics, and the independent t-test was employed for inferential statistics.
Results: The majority of elderly people participating in the study were male (60.9%). Their mean (SD) age was 77 (5.9) years, and their mean (SD) length of stay in the nursing home was 14.38 (3.7) years. The mean (SD) quality of life score for all elderly people investigated was 44.32 (13.90) out of 93. Moreover, the mean (SD) quality of life score was significantly higher in men (51.86 [12.45]) compared to women (32.58 [5.10]) (p < 0.001).
Conclusion: Based on the results obtained, the quality of life among elderly people residing in nursing homes in Zanjan was found to be poor to moderate. Hence, it is recommended that relevant authorities and stakeholders consider implementing financial support and programs aimed at improving the quality of elderly people’s place of residence, in order to enhance their quality of life and the quality of care provided.
Objectives: The present research aimed to determine and compare the quality of life in elderly men and women residing in nursing homes.
Methods: This cross-sectional study was conducted on 110 elderly men and women residing in nursing homes in Zanjan province. Sampling was carried out through a convenience sampling method. The tools used in this study comprised a demographic information questionnaire and the Leiden-Padua (LEIPAD) Quality of Life Questionnaire. Data were analyzed using SPSS 20 software. The mean (standard deviation [SD]) and frequency (percentage) were used for descriptive statistics, and the independent t-test was employed for inferential statistics.
Results: The majority of elderly people participating in the study were male (60.9%). Their mean (SD) age was 77 (5.9) years, and their mean (SD) length of stay in the nursing home was 14.38 (3.7) years. The mean (SD) quality of life score for all elderly people investigated was 44.32 (13.90) out of 93. Moreover, the mean (SD) quality of life score was significantly higher in men (51.86 [12.45]) compared to women (32.58 [5.10]) (p < 0.001).
Conclusion: Based on the results obtained, the quality of life among elderly people residing in nursing homes in Zanjan was found to be poor to moderate. Hence, it is recommended that relevant authorities and stakeholders consider implementing financial support and programs aimed at improving the quality of elderly people’s place of residence, in order to enhance their quality of life and the quality of care provided.
Full-Text [PDF 777 kb]
(555 Downloads)
| | Full-Text (HTML) (132 Views)
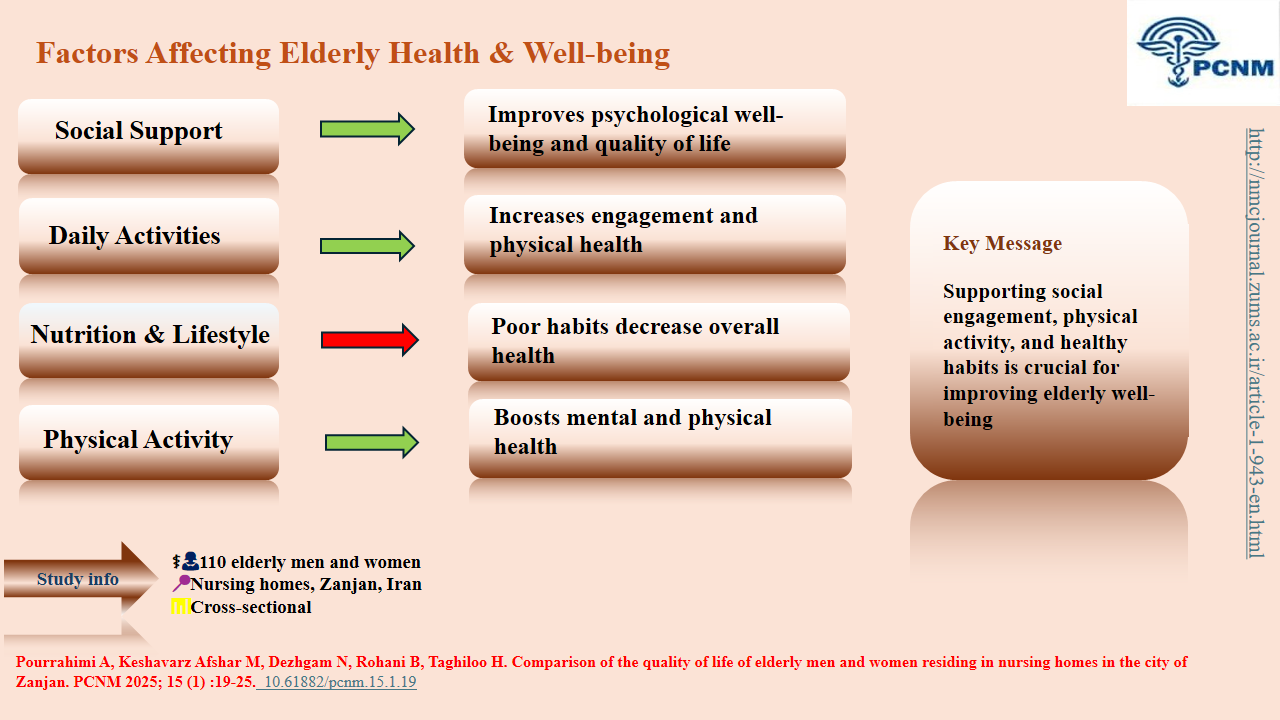
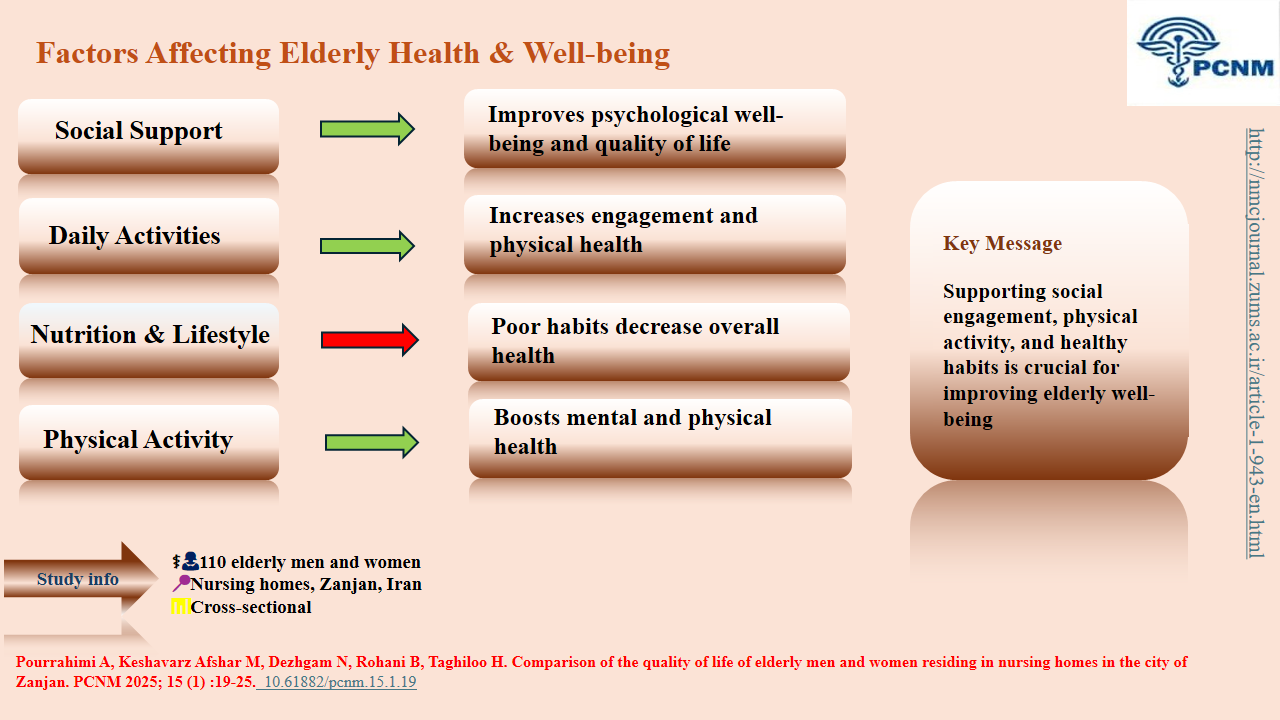
Knowledge Translation Statement
Audience: Nursing home managers, geriatric care planners, and health policymakers.
Elderly women in nursing homes experience a significantly lower quality of life than men, especially in physical and mental health. Care programs must be gender-sensitive, with targeted support for women's unique needs, to effectively improve well-being for all residents.
Type of Study: Orginal research |
Subject:
Nursing
References
1. Jadidi A, Farahaninia M, Janmohammadi S, Haghani H. The Relationship between Spiritual Well-Being and Quality of Life among Elderly People Residing in Kahrizak Senior House. Iran Journal of Nursing. 2011;24(72). [http://ijn.ir/article-1-922-en.html]
2. Ahmadi F, Takarli F, Farhadian M, Khoshbakht R, Shafiee A. The effect of group reminiscence on the quality of life in elderly. Scientific Journal of Nursing, Midwifery and Paramedical Faculty. 2022;8(1):35-49. [http://sjnmp.muk.ac.ir/article-۱-۴۷۶-fa.html]
3. Jazayeri E, Kazemipour S, Hosseini SR, Radfar M. Quality of life in the elderly: A community study. Caspian Journal of Internal Medicine. 2023;14(3):534. [https://doi.org/10.22088/cjim.14.3.543] [PMID]
4. Mokhtari F, Ghasemi N. Comparison of elderly's quality of life and mental health living in nursing homes and members of retiered club of Shiraz city. Iranian Journal of Ageing. 2011;5(4). [https://salmandj.uswr.ac.ir/article-A-10-278-7-1-en.html]
5. Rostami A, Heravi-Karimooi M. Quality of life of elderly during the covid-19 pandemic. Payesh (Health Monitor). 2023;22(1):83-93. [https://doi.org/10.52547/payesh.22.1.83]
6. Jangi Jahantigh L, Latifi Z, Soltani Zadeh M. The Effectiveness of Self-Healing Education on the Quality of Life in the Elderly. Aging Psychology. 2021;7(4):359-45. [https://doi.org/10.22126/jap.2022.6911.1561]
7. Teasdale MR. Quality of life and mission. Missiology. 2016;44(3):269-80. [https://doi.org/10.1177/0091829616645135]
8. Niazi M, Shafaiei Moghadam E. Physical Activity and Quality of Life of the Elderly. Iranian Journal of Culture and Health Promotion. 2022;6(3):457-63. [http://ijhp.ir/article-1-545-en.html]
9. Rafii F, Naseh L, Yadegary M. Relationship between Self-efficacy and Quality of Life in Ostomates. Iran Journal of Nursing. 2012;25(76). [http://ijn.ir/article-1-1128-en.html]
10. Maghsoudi A, Koohshoorinia Y, Hoseini M, Karami P, Atbaee M, Bahadori Z, et al. Comparison of quality of life among elderly people living in homes and nursing homes in Lar. Sadra Medical Journal. 2017;5(3):119-29. [https://smsj.sums.ac.ir/article_43925_en.html]
11. Shokouhi F, Tavassoli E, Amiripour A, Kaviani F. Quality of life of elderly living in nursing homes in Shahrekord. Scientific Journal of Nursing, Midwifery and Paramedical Faculty. 2020;5(4):84-93. [http://sjnmp.muk.ac.ir/article-1-297-en.html]
12. Riahi ME, Aliverdinia A, Pourhossein Z. Relationship between Social Support and Mental Health. Social Welfare. 2011;10(39):85-121. [http://refahj.uswr.ac.ir/article-1-322-en.html]
13. Khodaveisi M, Faal Araghi Nejad A, Omidi A, Esmaili Vardanjani A, Tapak L. Comparing the Structural Standards of Nursing Homes in Markazi Province, Iran With International Standards. Salmand: Iranian Journal of Ageing. 2018;13(3):362-71. [https://doi.org/10.32598/sija.13.3.362]
14. Ghadampour E, Heidaryani L, Radmehr F. Investigating the relationship between the meaning of life and self-esteem with the quality of life of the elderly living in the home and living in the nursing home. Avicenna Journal of Nursing and Midwifery Care. 2018;26(5):315-22. [https://doi.org/10.30699/sjhnmf.26.a5.315]
15. Barghi Irani Z, Ranjbar S. The Lived Experiences of Older Adults in Nursing Homes: A Phenomenological Study. Aging Psychology. 2024;10(1):127-11. [https://doi.org/10.22126/jap.2024.10330.1763]
16. Tajvar M, Arab M, Montazeri A. Determinants of health-related quality of life in elderly in Tehran, Iran. BMC Public Health. 2008;8(1):1-8. [https://doi.org/10.1186/1471-2458-8-323] [PMID]
17. Garrido A, Jentoft C, Ferrer JR V, JC AH, Marín G, Rego ADM. Quality of life in noninstitutionalized persons older than 65 years in two health care districts in Madrid. Atencion Primaria. 2003;31(5):285-92; discussion 93. [https://doi.org/10.1016/S0212-6567(03)79180-X]
18. Naseh L, Ali Sheikhi R, Rafii F. Quality of life and its related factors among elderlies living in nursing homes. Iran Journal of Nursing (IJN). 2014;27(87). [https://doi.org/10.29252/ijn.27.87.67]
19. De Leo D, Diekstra RFW, Lonnqvist J, Lonnqvist J, Cleiren M, Frisoni G, et al. LEIPAD, an internationally applicable instrument to assess quality of life in the elderly. Behavioral Medicine. 1998;24(1):17-27. [https://doi.org/10.1080/08964289809596377] [PMID]
20. Ghasemi H, Harirchi M, Masnavi A, Rahgozar M, Akbarian M. Comparing quality of life between seniors living in families and institutionalized in nursing homes. Social Welfare Quarterly. 2011;10(39):177-200. [http://refahj.uswr.ac.ir/article-1-346-en.html]
21. Hesamzadeh A, Maddah SB, Mohammadi F, Fallahi Khoshknab M, Rahgozar M. Comparison of elderlys" quality of life" living at homes and in private or public nursing homes. Iranian Journal of Ageing. 2010;4(4). [http://salmandj.uswr.ac.ir/article-1-307-en.html]
22. Ogunbode AM, Adebusoye LA, Olowookere OO, Owolabi M, Ogunniyi A. Factors associated with insomnia among elderly patients attending a geriatric centre in Nigeria. Current Gerontology and Geriatrics Research. 2014;2014. [https://doi.org/10.1155/2014/780535] [PMID]
23. Karmakar N, Datta A, Nag K, Tripura K. Quality of life among geriatric population: A cross-sectional study in a rural area of Sepahijala District, Tripura. Indian Journal of Public Health. 2018;62(2):95. [https://doi.org/10.4103/ijph.IJPH_121_17] [PMID]
24. Dehesh M, Rejeh N, Tadrisi SD, Tayebi A. Fear of Falls and Related Factors in The Elderly Undergoing Dialysis Referred to Hospitals in Tehran 2021. Qom University of Medical Sciences Journal. 2021;15(9):640-9. [https://doi.org/10.32598/qums.15.9.2466.1]
25. Prochota B, Szwamel K, Uchmanowicz I. Socio-clinical variables affecting the level of self-care in elderly patients with heart failure. European Journal of Cardiovascular Nursing. 2019;18(7):628-36. [https://doi.org/10.1177/1474515119855600] [PMID]
26. Aliasquarpoor M, Eybpoosh S. The quality of life of elderly nursing home residents and its relationship with different factors. Iran Journal of Nursing. 2012;25(75):60-70. [http://ijn.ir/article-1-1196-en.html]
27. Pachana NA, McLaughlin D, Leung J, Byrne G, Dobson A. Anxiety and depression in adults in their eighties: do gender differences remain? International Psychogeriatrics. 2012;24(1):145-50. [https://doi.org/10.1017/S1041610211001372] [PMID]
28. Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey I: Lifetime prevalence, chronicity and recurrence. Journal of Affective Disorders. 1993;29(2-3):85-96. [https://doi.org/10.1016/0165-0327(93)90026-G]
29. Van't Veer-Tazelaar PJN, Van Marwijk HW, Jansen APD, Rijmen F, Kostense PJ, Van Oppen P, et al. Depression in old age (75+), the PIKO study. Journal of Affective Disorders. 2008;106(3):295-9. [https://doi.org/10.1016/j.jad.2007.07.004] [PMID]
30. Aartsen MJ, Martin M, Zimprich D. Gender differences in level and change in cognitive functioning. Gerontology. 2004;50(1):35-8. [https://doi.org/10.1159/000074387] [PMID]
31. Gur RC, Mozley PD, Resnick SM, Gottlieb GL, Kohn M, Zimmerman R, et al. Gender differences in age effect on brain atrophy measured by magnetic resonance imaging. Proceedings of the National Academy of Sciences. 1991;88(7):2845-9. [https://doi.org/10.1073/pnas.88.7.2845] [PMID]
32. Fritsch T, McClendon MJ, Smyth KA, Lerner AJ, Friedland RP, Larsen JD. Cognitive functioning in healthy aging: the role of reserve and lifestyle factors early in life. The Gerontologist. 2007;47(3):307-22. [https://doi.org/10.1093/geront/47.3.307] [PMID]
33. Kontula O, Haavio-Mannila E. The impact of aging on human sexual activity and sexual desire. Journal of Sex Research. 2009;46(1):46-56. [https://doi.org/10.1080/00224490802624414] [PMID]
34. DeLamater J, Karraker A. Sexual functioning in older adults. Current Psychiatry Reports. 2009;11(1):6-11. [https://doi.org/10.1007/s11920-009-0002-4]
35. Hatfield EC, Luckhurst C, Rapson RL. Sexual motives: The impact of gender, personality, and social context on sexual motives and sexual behavior-Especially risky sexual behavior. Interpersona: An International Journal on Personal Relationships. 2011;5(2):95-133. [https://doi.org/10.5964/ijpr.v5i2.60]
36. Sujarwoto S, Tampubolon G, Pierewan AC. Individual and contextual factors of happiness and life satisfaction in a low middle income country. Applied Research in Quality of Life. 2018;13(4):927-45. [https://doi.org/10.1007/s11482-017-9567-y]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




