
Preventive Care in Nursing and Midwifery Journal

Volume 15, Issue 1 (1-2025)
Prev Care Nurs Midwifery J 2025, 15(1): 30-36 |
Back to browse issues page
Ethics code: 400.14.5.4/13.248/102.9/2024
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nikentari L A, Kristianto H, Yuliatun L, Haedar A, Irawan P L T. Blood glucose and neurological status: Dual predictors of survival in diabetic emergencies. Prev Care Nurs Midwifery J 2025; 15 (1) :30-36
URL: http://nmcjournal.zums.ac.ir/article-1-944-en.html
URL: http://nmcjournal.zums.ac.ir/article-1-944-en.html
Lintang Arum Nikentari 

 , Heri Kristianto *
, Heri Kristianto * 

 , Laily Yuliatun
, Laily Yuliatun 

 , Ali Haedar
, Ali Haedar 

 , Paulus Lucky Tirma Irawan
, Paulus Lucky Tirma Irawan 




 , Heri Kristianto *
, Heri Kristianto * 

 , Laily Yuliatun
, Laily Yuliatun 

 , Ali Haedar
, Ali Haedar 

 , Paulus Lucky Tirma Irawan
, Paulus Lucky Tirma Irawan 


Nursing Department, Faculty of Health Sciences, Brawijaya University, Malang, Indonesia , heri.kristianto@ub.ac.id
Abstract: (1113 Views)
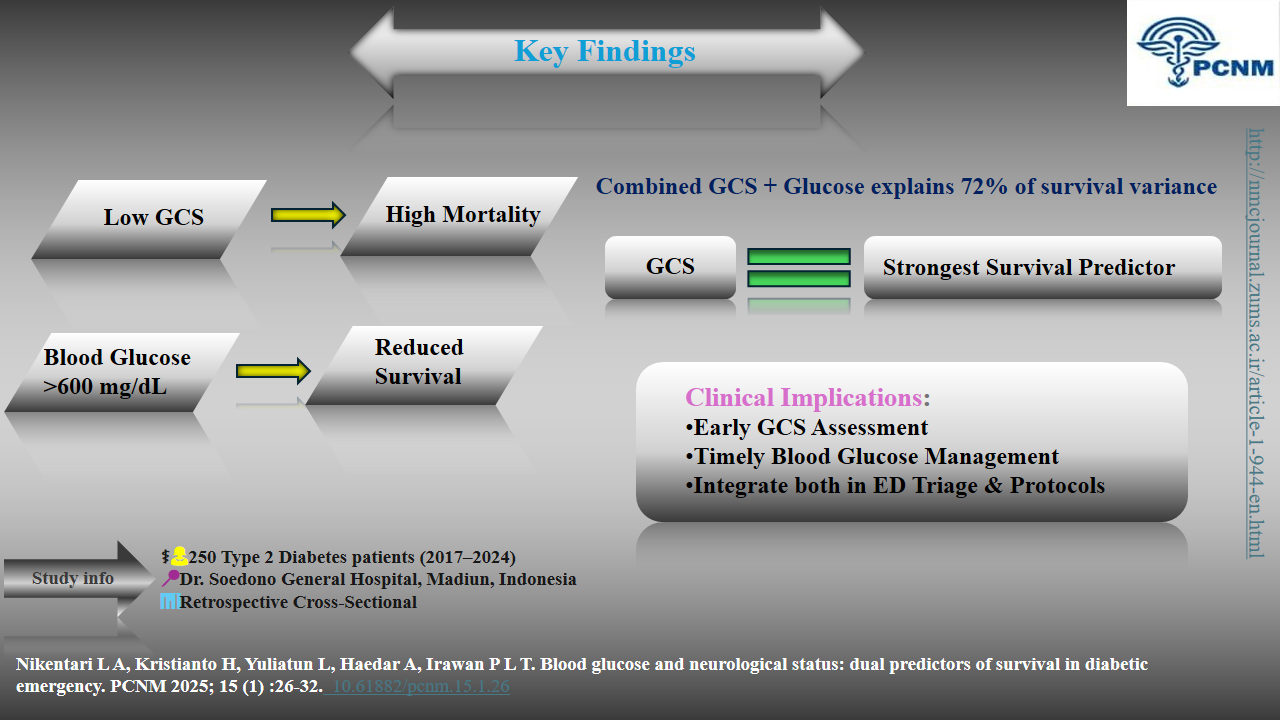
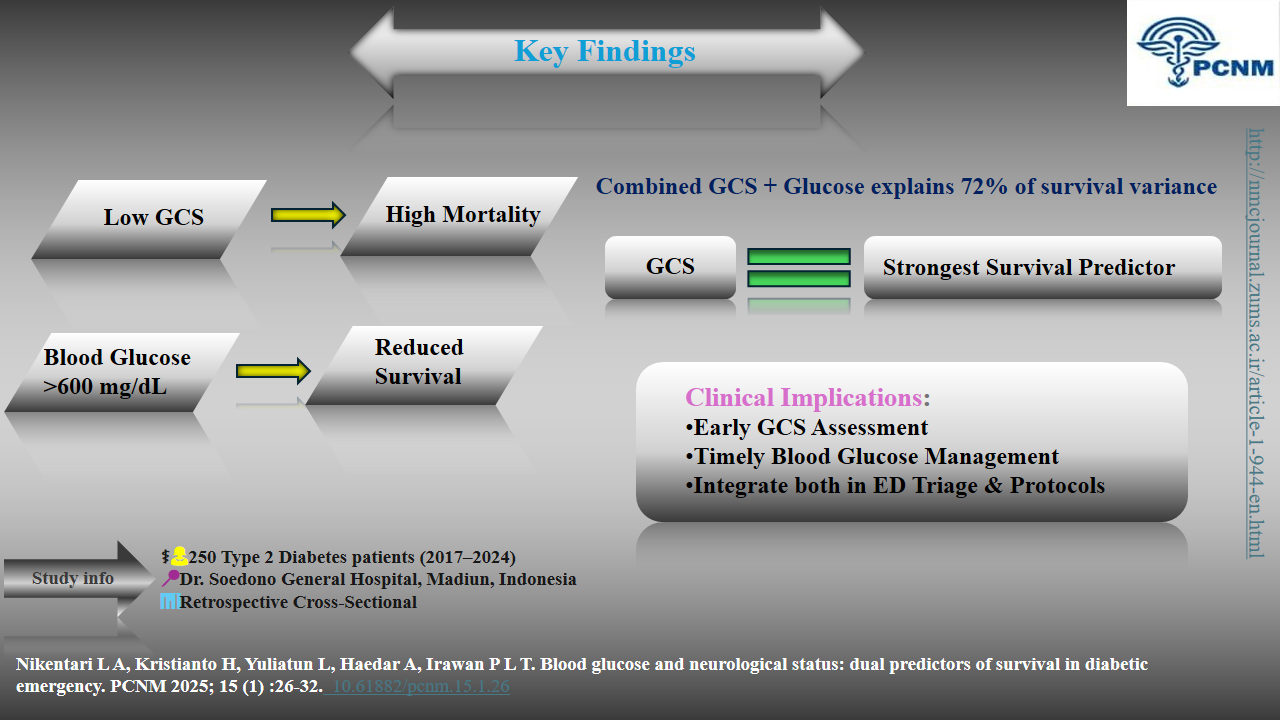
Background: Acute diabetic emergencies, including diabetic ketoacidosis (DKA), hyperosmolar hyperglycaemic syndrome (HHS), and hypoglycaemia, require urgent medical intervention. These complications result from severe metabolic disturbances, often causing neurological impairment. Blood glucose levels measure metabolic derangement, while the Glasgow Coma Scale (GCS) indicates cerebral dysfunction.
Objectives: This study evaluates the prognostic significance of blood glucose levels and GCS in predicting survival rates among diabetic emergency patients, hypothesizing that these parameters are robust outcome indicators.
Methods: A retrospective cross-sectional study analysed medical records of 250 patients treated for diabetic emergencies at Dr. Soedono General Hospital Madiun (2017–2024). Blood glucose levels and GCS scores were assessed using chi-square tests (p < 0.25) and multivariate binomial logistic regression (p < 0.05) in SPSS version 21.
Results: Multivariate analysis identified GCS as the most critical survival predictor, with low GCS scores significantly correlating with mortality (OR = 0.002, 95% CI: 0.000–0.012, p < 0.05). Blood glucose levels >600 mg/dL were also associated with reduced survival rates (OR = 0.113, 95% CI: 0.074–4.304, p < 0.05). The model explained 72.1% of the variance in patient outcomes.
Conclusion: GCS and blood glucose levels are pivotal survival predictors in diabetic emergencies, with GCS being the predominant determinant. These findings highlight the importance of early neurological evaluation and glucose regulation in improving outcomes.
Objectives: This study evaluates the prognostic significance of blood glucose levels and GCS in predicting survival rates among diabetic emergency patients, hypothesizing that these parameters are robust outcome indicators.
Methods: A retrospective cross-sectional study analysed medical records of 250 patients treated for diabetic emergencies at Dr. Soedono General Hospital Madiun (2017–2024). Blood glucose levels and GCS scores were assessed using chi-square tests (p < 0.25) and multivariate binomial logistic regression (p < 0.05) in SPSS version 21.
Results: Multivariate analysis identified GCS as the most critical survival predictor, with low GCS scores significantly correlating with mortality (OR = 0.002, 95% CI: 0.000–0.012, p < 0.05). Blood glucose levels >600 mg/dL were also associated with reduced survival rates (OR = 0.113, 95% CI: 0.074–4.304, p < 0.05). The model explained 72.1% of the variance in patient outcomes.
Conclusion: GCS and blood glucose levels are pivotal survival predictors in diabetic emergencies, with GCS being the predominant determinant. These findings highlight the importance of early neurological evaluation and glucose regulation in improving outcomes.
Keywords: Diabetic Ketoacidosis, Glasgow Coma Scale, Hyperosmolar Hyperglycemic Syndrome, Blood Glucose, Emergency Care
Full-Text [PDF 1024 kb]
(745 Downloads)
| | Full-Text (HTML) (36 Views)
Knowledge Translation Statement
Audience: Emergency Department managers, emergency nurses, and clinical policymakers.
In diabetic emergencies, a low Glasgow Coma Scale (GCS) score is the strongest predictor of mortality, even more critical than extreme blood glucose levels. Triage protocols must prioritize immediate neurological assessment alongside glucose management to identify high-risk patients and guide life-saving interventions.
Knowledge Translation Statement
Audience: Emergency Department managers, emergency nurses, and clinical policymakers.
In diabetic emergencies, a low Glasgow Coma Scale (GCS) score is the strongest predictor of mortality, even more critical than extreme blood glucose levels. Triage protocols must prioritize immediate neurological assessment alongside glucose management to identify high-risk patients and guide life-saving interventions.
Type of Study: Orginal research |
Subject:
Nursing
References
1. Saifullah H. Diabetic emergency: diabetic ketoacidosis, hyperglycemic hyperosmolar state, euglycemic diabetic ketoacidosis and hypoglycemia. International Journal of Contemporary Research. 2024;3(1):31-37. [https://multiarticlesjournal.com/counter/d/3-1-7/IJCRM-2024-3-1-7.pdf.]
2. Rusdi MS. Hipoglikemia pada pasien diabetes melitus. Journal Syifa Science and Clinical Research. 2020;2(September):83-90. [https://doi.org/10.37311/jsscr.v2i2.4575]
3. Muneer M, Akbar I. Acute metabolic emergencies in diabetes: DKA, HHS and EDKA. Advances in Experimental Medicine and Biology. 2021;1307:85-114. [https://doi.org/10.1007/5584_2020_545] [PMID]
4. Lotter N, Lahri S, van Hoving DJ. The burden of diabetic emergencies on the resuscitation area of a district-level public hospital in Cape Town. African Journal of Emergency Medicine. 2021;11(4):416-421. [https://doi.org/10.1016/j.afjem.2021.05.004] [PMID]
5. Braine ME, Cook N. The Glasgow coma scale and evidence-informed practice: a critical review of where we are and where we need to be. Journal of Clinical Nursing. 2017;26(1-2):280-293. [https://doi.org/10.1016/j.afjem.2021.05.004] [PMID]
6. Pawils S, Heumann S, Schneider SA, Metzner F, Mays D. The current state of international research on the effectiveness of school nurses in promoting the health of children and adolescents: an overview of reviews. PLOS One. 2023;18(4). [https://doi.org/10.1371/journal.pone.0275724] [PMID]
7. Sarang B, Bhandarkar P, Raykar N, O'Reilly GM, Soni KD, Wärnberg MG, et al. Associations of on-arrival vital signs with 24-hour in-hospital mortality in adult trauma patients admitted to four public university hospitals in urban India: a prospective multi-centre cohort study. Injury. 2021;52(5):1158-1163. [https://doi.org/10.1016/j.injury.2021.02.075] [PMID]
8. Akram Z, Inayat M, Akhtar S, Perveen R, Saeed R, Abid J, et al. Fasting influence on diabetic emergency visits in a tertiary care hospital throughout Ramadan and other lunar months. Pakistan Journal of Medical and Health Sciences. 2023;17(3):588-590. [https://doi.org/10.53350/pjmhs2023173588]
9. Maharjan J, Pandit S, Johansson KA, Khanal P, Karmacharya B, Kaur G, et al. Effectiveness of interventions for emergency care of hypoglycaemia and diabetic ketoacidosis: a systematic review. Diabetes Research and Clinical Practice. 2024;207. [https://doi.org/10.1016/j.diabres.2023.111078] [PMID]
10. Tamzil R, Yaacob N, Noor N, Baharuddin K. Comparing the clinical effects of balanced electrolyte solutions versus normal saline in managing diabetic ketoacidosis: a systematic review and meta-analyses. Turkish Journal of Emergency Medicine. 2023;23(3):131-138. [https://doi.org/10.4103/tjem.tjem_355_22] [PMID]
11. Blank SP, Blank RM, Ziegenfuss MD. The importance of hyperosmolarity in diabetic ketoacidosis. Diabetic Medicine. 2020;37(12):2001-2008. [https://doi.org/10.1111/dme.14277] [PMID]
12. Watta R, Masi G, Katuuk ME. Screening faktor resiko diabetes melitus pada individu dengan riwayat keluarga diabetes melitus di RSUD Jailolo. Jurnal Keperawatan. 2020;8(1):44. [https://doi.org/10.35790/jkp.v8i1.28410]
13. Chen J, Zeng H, Ouyang X, Zhu M, Huang Q, Yu W, et al. The incidence, risk factors, and long-term outcomes of acute kidney injury in hospitalized diabetic ketoacidosis patients. BMC Nephrology. 2020;21(1):1-9. [https://doi.org/10.1186/1471-2369-7-1] [PMID]
14. Banday MZ, Sameer AS, Nissar S. Pathophysiology of diabetes: an overview. Avicenna Journal of Medicine. 2020;10(4):174-188. [https://doi.org/10.4103/ajm.ajm_53_20] [PMID]
15. Gelaw NB, Muche AA, Alem AZ, Gebi NB, Chekol YM, Tesfie TK, et al. Development and validation of risk prediction model for diabetic neuropathy among diabetes mellitus patients at selected referral hospitals, in Amhara regional state Northwest Ethiopia, 2005-2021. PLOS One. 2023;18(8):e0276472. [https://doi.org/10.1371/journal.pone.0276472] [PMID]
16. Wu XY, She DM, Wang F, Guo G, Li R, Fang P, et al. Clinical profiles, outcomes and risk factors among type 2 diabetic inpatients with diabetic ketoacidosis and hyperglycemic hyperosmolar state: a hospital-based analysis over a 6-year period. BMC Endocrine Disorders. 2020;20(1):1-9. [https://doi.org/10.1186/s12902-020-00659-5] [PMID]
17. Katuuk ME, Sitorus R, Sukmarini L. Penerapan teori self care Orem dalam asuhan keperawatan pasien diabetes melitus. Jurnal Keperawatan. 2020;8(1):1-22. [https://doi.org/10.35790/jkp.v8i1.28405]
18. Barski L, Golbets E, Jotkowitz A, Schwarzfuchs D. Management of diabetic ketoacidosis. European Journal of Internal Medicine. 2023;117:38-44. [https://doi.org/10.1016/j.ejim.2023.07.005] [PMID]
19. Jitraknatee J, Ruengorn C, Nochaiwong S. Prevalence and risk factors of chronic kidney disease among type 2 diabetes patients: a cross-sectional study in primary care practice. Scientific Reports. 2020;10(1):1-10. [https://doi.org/10.1038/s41598-020-63443-4] [PMID]
20. Dhatariya KK. The management of diabetic ketoacidosis in adults-an updated guideline from the Joint British Diabetes Society for Inpatient Care. Diabetic Medicine. 2022;39(6):e14788. [https://doi.org/10.1111/dme.14788] [PMID]
21. Wu F, Wu C, Wu Q, Yan F, Xiao Y, Du C. Prediction of death in intracerebral hemorrhage patients after minimally invasive surgery by vital signs and blood glucose. World Neurosurgery. 2024;184:e84-e94. [https://doi.org/10.1016/j.wneu.2024.01.061] [PMID]
22. Mohajan D, Mohajan HK. Hypoglycaemia among diabetes patients: a preventive approach. Journal of Innovative Medical Research. 2023;2(9):29-35. [https://doi.org/10.56397/JIMR/2023.09.05]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |

