Preventive Care in Nursing and Midwifery Journal

Volume 15, Issue 3 (7-2025)
Prev Care Nurs Midwifery J 2025, 15(3): 50-60 |
Back to browse issues page
Ethics code: IR.SSU.REC.1398.070.
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hosseini S E, setavand M, javadi M. Explaining the competencies required for intensive care unit nurses: A delphi study. Prev Care Nurs Midwifery J 2025; 15 (3) :50-60
URL: http://nmcjournal.zums.ac.ir/article-1-972-en.html
URL: http://nmcjournal.zums.ac.ir/article-1-972-en.html
Assistant professor, Department of Medical- Surgical Nursing, School of Nursing & Midwifery, Iran University of Medical Sciences, Tehran, Iran , esmat.hosseini_110@yahoo.com
Abstract: (494 Views)
Background: Rapid changes in the healthcare system necessitate the provision of high-quality and safe nursing care, a long-standing goal in nursing that depends on maintaining competence throughout the process.
Objectives: This study aimed to determine the clinical competencies of nurses in the intensive care unit.
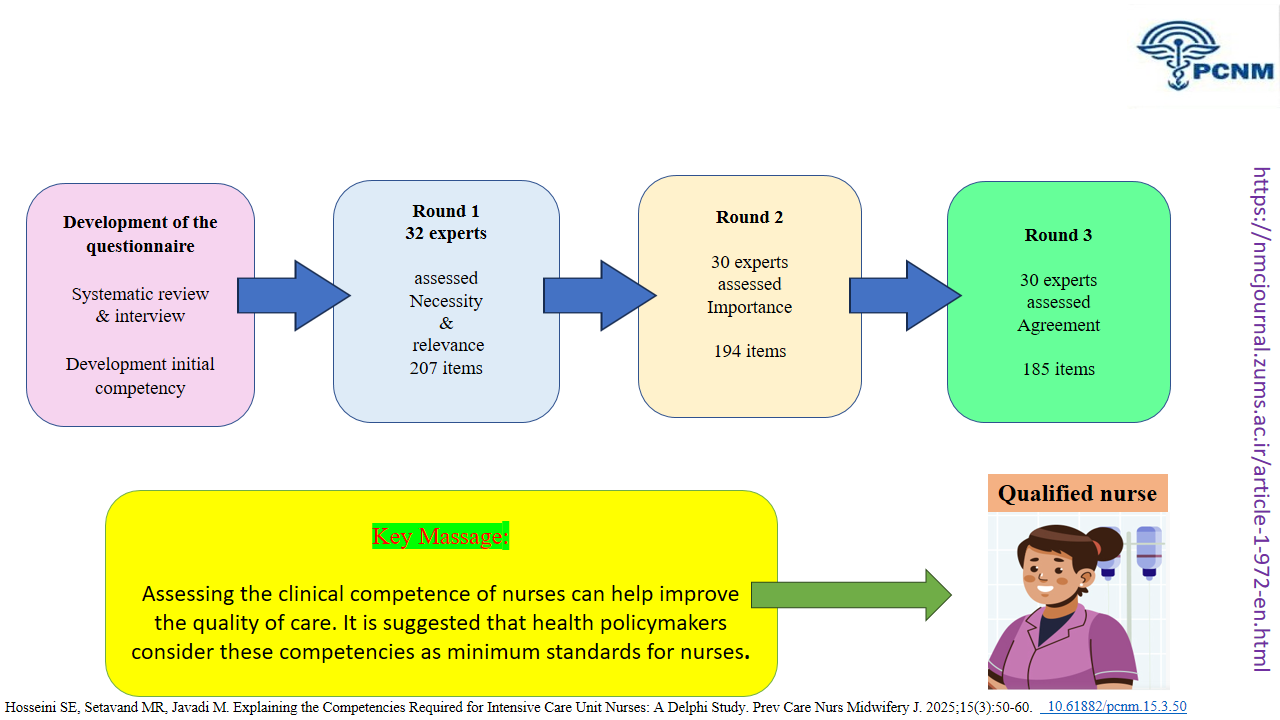
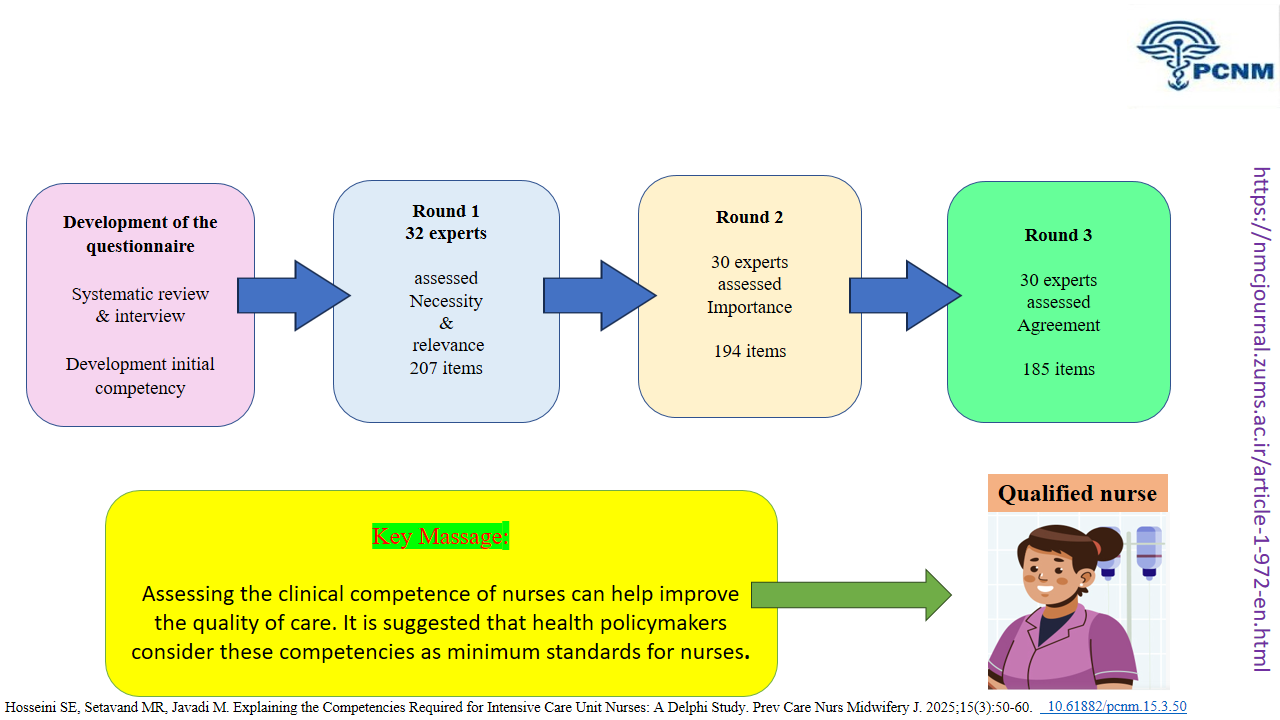
Methods: This study, conducted in three rounds using the Delphi method, selected 32 participants for participation through purposive sampling. In the first round, items were rated for necessity and relevance using 3- and 4-point Likert scales, respectively. Items that achieved ≥75% agreement, a mean score of ≥2.25 for necessity, and ≥3.0 for relevance were retained. In the second round, participants rated the importance of each item on a 4-point scale, and items with a mean score of ≥3.0 were included in the third round. In the final round, agreement was assessed on a two-way scale (agree = 1, disagree = 0), and items with a mean agreement score ≥0.75 (with 75% consensus) were considered final.
Results: A three-round Delphi study was conducted with 30 expert panelists (retention rate: 93.75%). Through systematic consensus-building, 185 competency items across 17 distinct domains were validated. The final framework encompasses critical areas such as personality traits, evidence-based care, patient safety, professionalism, communication, critical thinking, professional development, cultural/spiritual competence, and documentation. These domains demonstrated robust consensus, with mean relevance and importance scores ≥3.9 and agreement levels ≥97%. The competency framework achieved a high level of expert endorsement, with no items eliminated in the final round, confirming its comprehensiveness and contextual relevance for ICU nursing practice.
Conclusion: Assessing the clinical competence of nurses can help improve the quality of care. It is suggested that health policymakers consider these competencies as minimum standards for nurses.
Objectives: This study aimed to determine the clinical competencies of nurses in the intensive care unit.
Methods: This study, conducted in three rounds using the Delphi method, selected 32 participants for participation through purposive sampling. In the first round, items were rated for necessity and relevance using 3- and 4-point Likert scales, respectively. Items that achieved ≥75% agreement, a mean score of ≥2.25 for necessity, and ≥3.0 for relevance were retained. In the second round, participants rated the importance of each item on a 4-point scale, and items with a mean score of ≥3.0 were included in the third round. In the final round, agreement was assessed on a two-way scale (agree = 1, disagree = 0), and items with a mean agreement score ≥0.75 (with 75% consensus) were considered final.
Results: A three-round Delphi study was conducted with 30 expert panelists (retention rate: 93.75%). Through systematic consensus-building, 185 competency items across 17 distinct domains were validated. The final framework encompasses critical areas such as personality traits, evidence-based care, patient safety, professionalism, communication, critical thinking, professional development, cultural/spiritual competence, and documentation. These domains demonstrated robust consensus, with mean relevance and importance scores ≥3.9 and agreement levels ≥97%. The competency framework achieved a high level of expert endorsement, with no items eliminated in the final round, confirming its comprehensiveness and contextual relevance for ICU nursing practice.
Conclusion: Assessing the clinical competence of nurses can help improve the quality of care. It is suggested that health policymakers consider these competencies as minimum standards for nurses.
Full-Text [PDF 758 kb]
(207 Downloads)
| | Full-Text (HTML) (149 Views)
Knowledge Translation Statement
Audience: ICU nurse managers, hospital nursing directors, clinical nurse educators, and policymakers in critical care
A Delphi study establishes that ICU nurse competency is a multi-dimensional construct requiring both advanced technical skills and essential non-technical skills in ethics, communication, and family care. To ensure a proficient workforce, healthcare institutions must develop and implement standardized, evidence-based competency frameworks that move beyond task-checklists to holistically assess and train nurses in this full spectrum of skills.
Audience: ICU nurse managers, hospital nursing directors, clinical nurse educators, and policymakers in critical care
A Delphi study establishes that ICU nurse competency is a multi-dimensional construct requiring both advanced technical skills and essential non-technical skills in ethics, communication, and family care. To ensure a proficient workforce, healthcare institutions must develop and implement standardized, evidence-based competency frameworks that move beyond task-checklists to holistically assess and train nurses in this full spectrum of skills.
Type of Study: Orginal research |
Subject:
Nursing
References
1. Tajari M, Ashktorab T, Ebadi A. Components of safe nursing care in the intensive care units: a qualitative study. BMC Nursing. 2024;23(1):613. [https://doi.org/10.1186/s12912-024-02180-9] [PMID]
2. Goñi-Viguria R. Experience of an advanced practice nurse in an intensive care unit. Enfermería Intensiva (English Edition). 2025;36(1):100482. [https://doi.org/10.1016/j.enfie.2025.100482] [PMID]
3. Zarei F, Dehghan M, Shahrbabaki PM. The relationship between perception of good death with clinical competence of end-of-life care in critical care nurses. OMEGA-Journal of Death and Dying. 2025;91(1):401-417.
https://doi.org/10.1177/00302228221134721 [https://doi.org/10.1177/00302228231155321] [PMID]
4. Pashaee S, Lakdizaji S, Rahmani A, Zamanzadeh V. Priorities of caring behaviors from critical care nurses viewpoints. Preventive Care in Nursing & Midwifery Journal. 2014;4(1):65-73. [http://pcnmj.mazums.ac.ir/article-1-155-en.html]
5. Perez-Gonzalez S, Marques-Sanchez P, Pinto-Carral A, Gonzalez-Garcia A, Liebana-Presa C, Benavides C. Characteristics of leadership competency in nurse managers: a scoping review. Journal of Nursing Management. 2024;2024(1):5594154. [https://doi.org/10.1155/2024/5594154] [PMID]
6. Coventry TH, Maslin-Prothero SE, Smith G. Organizational impact of nurse supply and workload on nurses continuing professional development opportunities: an integrative review. Journal of Advanced Nursing. 2015;71(12):2715-2727. [https://doi.org/10.1111/jan.12724] [PMID]
7. Bahreini M, Moattari M, Kaveh MH, Ahmadi F. A Comparison of Nurses' Clinical Competences in Two Hospitals Affiliated to Shiraz and Boushehr Universities of Medical Sciences: A Self-Assessment. Iranian Journal of Medical Education. 2010;10(2):155-163. [http://ijme.mui.ac.ir/article-1-1253-en.html]
8. Zaitoun RA. Assessing nurses' professional competency: a cross-sectional study in Palestine. BMC Nursing. 2024;23(1):379. [https://doi.org/10.1186/s12912-024-02064-y] [PMID]
9. Baik D, Yi N, Han O, Kim Y. Trauma nursing competency in the emergency department: a concept analysis. BMJ Open. 2024;14(6):e079259. [https://doi.org/10.1136/bmjopen-2023-079259] [PMID]
10. Rizany I, Hariyati RTS, Handayani H. Factors that affect the development of nurses' competencies: a systematic review. Enfermeria Clinica. 2018;28:154-157. [https://doi.org/10.1016/j.enfcli.2018.04.007] [PMID]
11. Almarwani AM, Alzahrani NS. Factors affecting the development of clinical nurses' competency: A systematic review. Nurse Education in Practice. 2023;73:103826. [https://doi.org/10.1016/j.nepr.2023.103826] [PMID]
12. Vafaee Najar A, Habashizade A, Karimi H, Ebrahimzade S. The effect of improvement of nursing managers' professional competencies based on performance on their productivity: An interventional study. Daneshvar Medicine. 2011;19(3):63-72. [http://daneshvarmed.shahed.ac.ir/article-1-456-en.html]
13. Kim HW, Kim MG. The relationship among academic achievement, clinical competence, and confidence in clinical performance of nursing students. The Journal of Korean Academic Society of Nursing Education. 2021;27(1):49-58. [https://doi.org/10.5977/jkasne.2021.27.1.49]
14. Le TTH, Aliswag EG. Quality of nursing care, compassionate care and patient satisfaction: A multiple regression in path analysis model. Journal of Nursing Science. 2025;8(01):17-28. [https://doi.org/10.54436/jns.2025.01.940]
15. Egerod I, Kaldan G, Nordentoft S, Larsen A, Herling SF, Thomsen T, et al. Skills, competencies, and policies for advanced practice critical care nursing in Europe: A scoping review. Nurse Education in Practice. 2021;54:103142. [https://doi.org/10.1016/j.nepr.2021.103142] [PMID]
16. Kaldan G, Nordentoft S, Herling SF, Larsen A, Thomsen T, Egerod I. Evidence characterising skills, competencies and policies in advanced practice critical care nursing in Europe: a scoping review protocol. BMJ Open. 2019;9(9):e031504. [https://doi.org/10.1136/bmjopen-2019-031504] [PMID]
17. Saqib M. Trends in Critical Care Medicine: Innovations Shaping the Future. In: Advances in Medical Technology. Springer; 2025:45-62. [https://doi.org/10.5772/intechopen.1010714]
18. Farsi Z, Nasiri M, Sajadi SA, Khavasi M. Comparison of Iran's nursing education with developed and developing countries: a review on descriptive-comparative studies. BMC Nursing. 2022;21(1):105. [https://doi.org/10.1186/s12912-022-00880-8] [PMID]
19. Keeney S, McKenna HP, Hasson F. The Delphi Technique in Nursing and Health Research. John Wiley & Sons; 2011. [https://doi.org/10.1002/9781444392029]
20. Jünger S, Payne SA, Brine J, Radbruch L, Brearley SG. Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: Recommendations based on a methodological systematic review. Palliative Medicine. 2017;31(8):684-706. [https://doi.org/10.1177/0269216317690685] [PMID]
21. Hohmann E, Beaufils P, Beiderbeck D, Chahla J, Geeslin A, Hasan S, et al. Guidelines for designing and conducting Delphi consensus studies: an expert consensus Delphi study. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2025;41(1):12-25. [https://doi.org/10.1016/j.arthro.2024.08.045] [PMID]
22. Shang Z. Use of Delphi in health sciences research: a narrative review. Medicine. 2023;102(7):e32829. [https://doi.org/10.1097/MD.0000000000032829] [PMID]
23. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15(9):1277-1288. [https://doi.org/10.1177/1049732305276687] [PMID]
24. Lim WM. What is qualitative research? An overview and guidelines. Australasian Marketing Journal. 2025;33(2):199-229. [https://doi.org/10.1177/14413582241264619]
25. del Pozo-Herce P, Martínez-Sabater A, Chover-Sierra E, Gea-Caballero V, Satústegui-Dordá PJ, Saus-Ortega C, et al. Application of the Delphi method for content validity analysis of a questionnaire to determine the risk factors of the Chemsex. Healthcare. 2023;11(5):742. [https://doi.org/10.3390/healthcare11050742] [PMID]
26. Najafi B, Nakhaei M. Clinical competence of nurses: a systematic review study. Journal of Nursing Education. 2022;11(2):45-56. [https://doi.org/10.21859/ijn-11025]
27. Yoo HJ, Lim OB, Shim JL. Critical care nurses' communication experiences with patients and families in an intensive care unit: A qualitative study. PLoS One. 2020;15(7):e0235694. [https://doi.org/10.1371/journal.pone.0235694] [PMID]
28. Nobahar M. Care quality in critical cardiac units from nurses perspective: A content analysis. Journal of Qualitative Research in Health Sciences. 2014;3(2):149-161. [http://jqr1.kmu.ac.ir/article-1-256-en.html]
29. Tunlind A, Granström J, Engström Å. Nursing care in a high-technological environment: Experiences of critical care nurses. Intensive and Critical Care Nursing. 2015;31(2):116-123. [https://doi.org/10.1016/j.iccn.2014.11.005] [PMID]
30. Kanjakaya P. Nurses perceptions regarding the use of technological equipment in the intensive care unit setting of a public sector hospital in Johannesburg [master's thesis]. University of the Witwatersrand; 2014. [http://wiredspace.wits.ac.za/handle/10539/15347]
31. O'Connell M, Reid B, O'Loughlin K. An exploration of the education and training experiences of ICU nurses in using computerised equipment. Australian Journal of Advanced Nursing. 2007;25(2):46-52. [https://search.informit.org/doi/10.3316/informit.838909887356254]
32. Santana-Padilla YG, Bernat-Adell MD, Santana-Cabrera L. Nurses' perception on competency requirement and training demand for intensive care nurses. International Journal of Nursing Sciences. 2022;9(3):350-356. [https://doi.org/10.1016/j.ijnss.2022.06.004] [PMID]
33. Bucknall TK. Critical care nurses' decision-making activities in the natural clinical setting. Journal of Clinical Nursing. 2000;9(1):25-36. [https://doi.org/10.1046/j.1365-2702.2000.00360.x] [PMID]
34. Thompson C, Aitken L, Doran D, Dowding D. An agenda for clinical decision making and judgement in nursing research and education. International Journal of Nursing Studies. 2013;50(12):1720-1726. [https://doi.org/10.1016/j.ijnurstu.2013.07.005] [PMID]
35. Hwang GJ, Cheng PY, Chang CY. Facilitating students' critical thinking, metacognition and problem-solving tendencies in geriatric nursing class: A mixed-method study. Nurse Education in Practice. 2025;83:104266. [https://doi.org/10.1016/j.nepr.2025.104266] [PMID]
36. Baharum H, Ismail A, McKenna L, Mohamed Z, Ibrahim R, Hassan NH. Success factors in adaptation of newly graduated nurses: a scoping review. BMC Nursing. 2023;22(1):125. [https://doi.org/10.1186/s12912-023-01279-9] [PMID]
37. Ortega-Lapiedra R, Barrado-Narvión MJ, Bernués-Oliván J. Acquisition of competencies of nurses: improving the performance of the healthcare system. International Journal of Environmental Research and Public Health. 2023;20(5):4510. [https://doi.org/10.3390/ijerph20054510] [PMID]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |